7 Deadly Signs of Coronary Artery Disease (CAD)
Understanding Coronary Artery Disease (CAD)
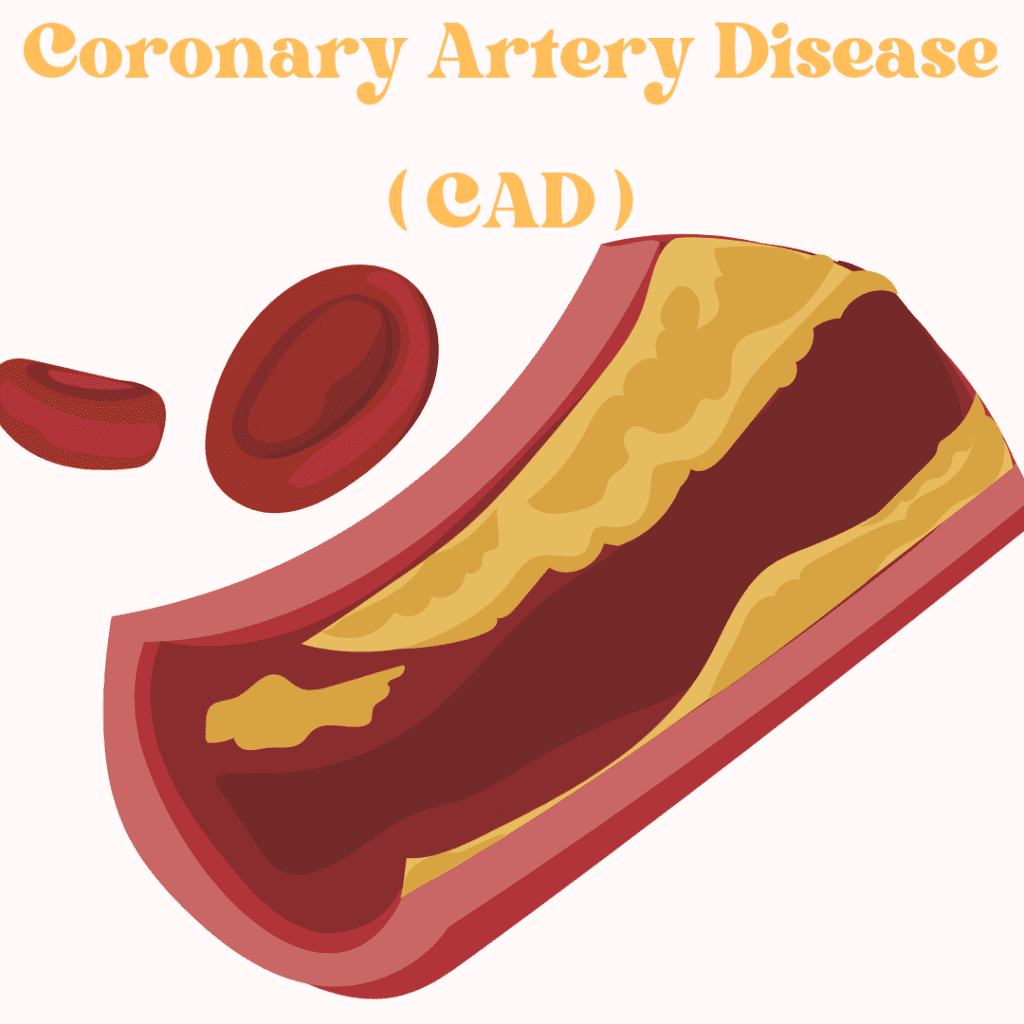
Coronary artery disease (CAD) is recognized as one of the most prevalent forms of cardiovascular disease worldwide, significantly contributing to morbidity and mortality rates across various populations. Its significance lies not only in the staggering numbers of individuals affected but also in its potential to lead to more severe conditions such as heart attacks and heart failure. At the core of CAD is the process of atherosclerosis, wherein plaque—a mixture of fat, cholesterol, and other substances—accumulates within the coronary arteries. This gradual buildup can lead to the narrowing of the arteries, ultimately restricting blood flow to the heart muscle.
As CAD progresses, the reduction in blood flow can lead to various symptoms, including chest pain, shortness of breath, and fatigue. In many cases, individuals may remain asymptomatic until an advanced stage of the disease is reached, underscoring the importance of early detection and intervention. Modifiable risk factors, including high LDL cholesterol levels, hypertension, diabetes, smoking, and a sedentary lifestyle, play a crucial role in the development of CAD. Hence, awareness and management of these factors are essential for prevention and effective treatment.
The impact of coronary artery disease extends beyond the individual, affecting families and communities through the burden of healthcare costs and loss of productivity. Given its global prevalence, CAD poses an urgent public health challenge that necessitates comprehensive strategies aimed at education, prevention, and treatment. Understanding the nature of CAD, including how it develops and the factors that influence its progression, is essential in addressing this condition and mitigating its health effects on the population. Following this introduction, further exploration of its causes, symptoms, treatments, and preventive measures will provide deeper insights into managing and combating this critical health issue.
Causes and Risk Factors of CAD
Coronary artery disease (CAD) primarily arises from the buildup of plaque in the coronary arteries, which supply blood to the heart muscle. Various factors contribute to the development of CAD, with some being controllable through lifestyle changes and others being inherent characteristics. Understanding these causes and risk factors is crucial for prevention and management.
High cholesterol levels play a significant role in the development of CAD. When there is too much low-density lipoprotein (LDL) cholesterol in the bloodstream, it can lead to plaque formation, which narrows and hardens the arteries. Regular monitoring and management of cholesterol levels through diet, exercise, and medication can help mitigate this risk.
Hypertension, or high blood pressure, is another major contributor. It puts added strain on the arteries and can accelerate the process of atherosclerosis, further increasing the likelihood of CAD. Maintaining a healthy blood pressure through lifestyle modifications and, if necessary, medications is vital for reducing cardiovascular risks.
Smoking is a critical risk factor often linked to numerous health conditions, including CAD. The toxins in cigarette smoke can damage blood vessels and promote plaque buildup. Quitting smoking, thus, can substantially decrease the risk of developing coronary artery disease.
Diabetes is also closely associated with an increased risk of CAD. Elevated blood sugar levels can lead to increased plaque formation. Proper management of diabetes and maintaining healthy blood sugar levels are essential in minimizing the threat of heart disease.
Obesity is another significant risk factor that contributes to other health issues, such as diabetes and hypertension, ultimately raising the likelihood of CAD. A balanced diet combined with regular physical activity can combat obesity and its related complications.
Lastly, genetic predisposition may play a considerable role in an individual’s risk for CAD. A family history of heart disease can indicate a higher chance of developing similar conditions. While this risk cannot be changed, awareness can promote proactive health measures to lower other contributing factors.
Symptoms of Coronary Artery Disease
Coronary artery disease (CAD) manifests through a range of symptoms, which can vary significantly among individuals. One of the hallmark symptoms is angina, characterized by chest pain or discomfort. This sensation often feels like pressure, squeezing, or a feeling of fullness in the chest, and it may also radiate to the shoulders, neck, arms, back, teeth, or jaw. Angina typically occurs during physical exertion or emotional stress, as increased activity requires more blood flow to the heart, which narrowed arteries can struggle to deliver.
Shortness of breath is another common symptom associated with CAD. This can occur during physical activities or even at rest in advanced stages of the disease. The inability to catch one’s breath can create significant distress and may indicate that the heart is not receiving adequate blood supply. Fatigue is also prevalent among those suffering from coronary artery disease, which can manifest as a persistent feeling of exhaustion unrelated to physical exertion. This symptom often goes unrecognized as a potential sign of heart issues, especially in women, who may experience atypical symptoms compared to men.
It is crucial to note that symptoms can differ widely among individuals. Some may experience debilitating chest pain, while others might only encounter mild discomfort or additional symptoms such as nausea, lightheadedness, or cold sweats. As CAD progresses, the severity and frequency of these symptoms may also escalate. Early recognition and prompt medical evaluation of these symptoms are vital for effective intervention. Individuals experiencing signs of coronary artery disease, particularly if they are new or have changed in intensity, should seek medical attention promptly for accurate diagnosis and appropriate management of their condition.

Diagnosis of Coronary Artery Disease
The diagnosis of coronary artery disease (CAD) comprises a series of evaluations that are essential for accurate identification and management of the condition. Initially, a healthcare provider will conduct a physical exam, which includes an assessment of the patient’s medical history, lifestyle factors, and any presenting symptoms such as chest pain or shortness of breath. This comprehensive approach allows for a focused inquiry into potential risk factors associated with CAD, including hypertension, diabetes, obesity, and high cholesterol levels.
Following the physical exam, blood tests play a crucial role in diagnosing coronary artery disease. These tests assess cholesterol levels, glucose levels, and other markers that may indicate an increased risk for heart disease. The information obtained from blood tests can inform treatment options and lifestyle modifications that may be necessary.
Electrocardiograms (ECG) are frequently employed to observe the electrical activity of the heart. An ECG can help detect irregularities in heart rhythm and identify past heart attacks, contributing valuable insights into a patient’s cardiac health. Another method, the echocardiogram, utilizes sound waves to create images of the heart. This imaging technique helps in assessing heart function and the status of heart valves, which may be affected by coronary artery disease.
Stress tests are another important diagnostic tool, wherein the patient’s heart is monitored while they engage in physical activity or during the administration of medication that simulates exercise. This procedure helps to determine how well the heart performs under stress, revealing potential blockages in the coronary arteries.
Lastly, coronary angiography serves as a definitive diagnostic method. This procedure involves the injection of contrast dye into the coronary arteries, allowing for the visualization of any blockages via X-ray imaging. The combination of these diagnostic tools provides a comprehensive understanding of coronary artery disease, enabling healthcare providers to formulate effective management strategies tailored to the individual needs of each patient.
Treatment Options for Coronary Artery Disease
Coronary artery disease (CAD) is often managed through a combination of lifestyle changes, medications, and, in some cases, surgical interventions. The treatment strategy for CAD must be personalized, taking into account the severity of the disease, risk factors, and individual patient needs. The primary goal of treatment is to reduce symptoms, improve heart function, and minimize the risk of heart attacks. Lifestyle modifications play a critical role in the overall management of CAD. These changes may include adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins, along with regular physical activity and weight management. Smoking cessation is equally vital, as tobacco use significantly contributes to the progression of coronary artery disease.
In addition to lifestyle changes, pharmacological treatments are commonly employed to manage CAD symptoms and reduce cardiovascular risks. Several classes of medications are utilized, including antiplatelet agents (such as aspirin), beta-blockers, statins, and ACE inhibitors. Antiplatelet agents help to prevent blood clots, while beta-blockers reduce the heart’s workload and blood pressure. Statins work by lowering cholesterol levels, thus slowing the progression of atherosclerosis, which is the primary cause of CAD.
For patients whose condition does not respond adequately to medication and lifestyle changes, surgical options may be considered. Percutaneous coronary intervention (PCI), also known as coronary angioplasty, involves the insertion of a catheter to open blocked arteries, often with a stent placement. In more severe cases, coronary artery bypass graft (CABG) surgery may be necessary, which involves redirecting blood flow around blocked arteries using blood vessels from other areas of the body. Ultimately, the choice of treatment for coronary artery disease should be made collaboratively between the patient and healthcare providers, ensuring that the management plan aligns with the patient’s overall health goals and preferences.
Lifestyle Changes for Prevention and Management
Coronary artery disease (CAD) is a leading cause of morbidity and mortality worldwide. Adopting specific lifestyle changes is critical in both preventing and managing this condition. A multifaceted approach, encompassing diet, exercise, smoking cessation, and stress management, has been shown to significantly mitigate the risk of CAD.
Dietary modifications are foundational for heart health. A heart-healthy diet should emphasize the consumption of fruits, vegetables, whole grains, lean proteins, and healthy fats, particularly those sourced from fish and nuts. Limiting saturated fats and trans fats can lower cholesterol levels and reduce arterial plaque buildup, which is essential for preventing coronary artery disease. The Mediterranean diet, rich in omega-3 fatty acids and antioxidants, has demonstrated efficacy in improving cardiovascular health and should be considered a model for dietary habits.
Physical activity is another crucial element in the prevention and management of CAD. Engaging in regular exercise—at least 150 minutes of moderate aerobic activity per week—helps bolster cardiovascular fitness, reduce weight, and improve overall heart health. Activities such as walking, cycling, and swimming can enhance blood flow and lower blood pressure, thereby reducing the risk of coronary artery disease.
Another significant lifestyle change involves smoking cessation. Smoking is a major risk factor for CAD and its cessation can lead to immediate improvements in heart health. Resources such as counseling, support groups, and nicotine replacement therapies can aid individuals in quitting smoking, ultimately reducing their risk and improving their overall wellbeing.
Finally, effective stress management is paramount in maintaining heart health. Chronic stress can lead to unhealthy coping mechanisms such as poor diet, inactivity, and smoking. Techniques including mindfulness, meditation, and yoga can help alleviate stress and promote a healthier lifestyle. By integrating these strategies, individuals can significantly reduce their risk of coronary artery disease and improve their overall cardiovascular health.

The Role of Nutrition in Heart Health
Nutrition plays a pivotal role in maintaining heart health and preventing coronary artery disease (CAD). A well-balanced diet can significantly reduce the risk factors associated with this common condition. One of the foremost dietary patterns recommended by healthcare professionals is the Mediterranean diet, which emphasizes whole grains, fruits, vegetables, legumes, fish, and healthy fats such as olive oil. This dietary approach is rich in beneficial nutrients and has been linked to improved cardiovascular outcomes.
A key element in maintaining heart health is the inclusion of omega-3 fatty acids, found primarily in fatty fish like salmon, as well as in flaxseeds and walnuts. Omega-3 fatty acids have anti-inflammatory properties and contribute to lowering blood triglyceride levels, which can reduce the risk of heart disease. Moreover, antioxidants, which can be found in a variety of fruits and vegetables, help combat oxidative stress and inflammation in the body. Nutrients such as vitamin C, vitamin E, and beta-carotene are particularly noted for their heart-protective qualities.
Maintaining a healthy weight is also crucial in minimizing the risk of CAD. Excess weight can contribute to high blood pressure, diabetes, and elevated cholesterol levels, all of which are significant risk factors for heart disease. Adopting a heart-healthy diet combined with regular physical activity can facilitate weight management and promote overall cardiovascular health.
When it comes to meal planning and grocery shopping, it is essential to prioritize whole and minimally processed foods. Creating a weekly menu that incorporates a variety of nutrient-dense foods can help individuals make healthier choices. Additionally, reading food labels and being mindful of portion sizes can aid in maintaining a heart-healthy diet.
By embracing a nutritious lifestyle focused on heart-healthy foods, individuals can take proactive steps toward reducing their risk of coronary artery disease and fostering long-term cardiovascular wellness.
Research and Innovations in CAD Treatment
As medical science progresses, the exploration of innovative treatments and technologies for coronary artery disease (CAD) continues to gather momentum. Recent advancements in medical technology and therapies are transforming the landscape of CAD management. Notably, the integration of advanced imaging techniques, such as intravascular ultrasound and optical coherence tomography, enables healthcare professionals to gain a deeper understanding of a patient’s arterial condition. These advanced modalities can identify blockages and abnormalities with greater precision, thereby facilitating tailored treatment plans.
Moreover, new medications targeting CAD are under extensive investigation. Novel antiplatelet agents, lipid-lowering therapies, and anti-inflammatory medications are being studied for their efficacy in managing this condition. One promising area of research involves the role of emerging drugs in stabilizing atherosclerotic plaques, which can significantly reduce the risk of heart attacks and other cardiovascular events. The ongoing exploration of gene therapies and regenerative medicine appears promising, as scientists are investigating their potential to restore normal function in damaged cardiac tissues.
In addition to pharmacological advancements, surgical techniques are also evolving. Minimally invasive procedures, such as robotic-assisted coronary artery bypass grafting and catheter-based interventions, are enhancing patient recovery times and reducing postoperative complications. These innovations are not only improving the quality of care for CAD patients but also expanding treatment options for those who may have previously been considered high-risk for traditional surgical interventions.
Crucially, clinical trials play an imperative role in developing and verifying these emerging treatment strategies. They provide vital insights into the safety and effectiveness of new therapies, ensuring that patients benefit from the latest scientific advancements. As research continues to unveil potential breakthroughs, both patients and healthcare providers must stay informed, fostering an environment of shared knowledge that can enhance decision-making and treatment outcomes in the fight against coronary artery disease.
FAQs about Coronary Artery Disease
Coronary artery disease (CAD) is a common condition that often raises various questions among individuals seeking to understand their heart health better. Below are some frequently asked questions that can help clarify common misconceptions about CAD.
What is the difference between CAD and heart disease?
Coronary artery disease is a specific type of heart disease that results from the narrowing or blockage of coronary arteries due to plaque buildup. This condition primarily affects the heart’s blood supply, leading to chest pain (angina) or even heart attacks. In contrast, “heart disease” is an umbrella term that encompasses a range of cardiovascular conditions, including CAD, heart rhythm disorders, and heart valve disease, among others. Understanding this distinction is crucial for effective prevention and management strategies.
How can I reduce my risk of CAD?
Reducing the risk of developing coronary artery disease involves adopting a heart-healthy lifestyle. Key strategies include maintaining a balanced diet low in saturated fats, cholesterol, and sodium while rich in fruits, vegetables, and whole grains. Regular physical activity, such as engaging in at least 150 minutes of moderate-intensity exercise each week, is also beneficial. Additionally, managing risk factors like hypertension, diabetes, and smoking cessation are vital steps. Regular check-ups with healthcare providers can foster a proactive approach to heart health.
What should I do if I suspect I have CAD?
If you harbor concerns regarding the possibility of having coronary artery disease, it is imperative to seek medical attention promptly. Initial steps typically involve a thorough evaluation by a healthcare professional, which may include a physical examination, blood tests, and imaging studies like an electrocardiogram (ECG) or a stress test. Early diagnosis and timely intervention are essential for improving outcomes and managing the condition effectively.
Can CAD be reversed or cured?
While coronary artery disease (CAD) cannot be completely cured, its progression can be slowed, halted, or even partially reversed with the right interventions. Lifestyle modifications such as a heart-healthy diet, regular exercise, smoking cessation, and stress management can help improve heart health. In some cases, medications like statins and procedures such as angioplasty or bypass surgery may be necessary to restore blood flow. Early detection and proactive management are key to preventing complications.
Are there any early warning signs of CAD?
Yes, CAD often presents with early warning signs that should not be ignored. These may include chest discomfort (angina), shortness of breath, fatigue, dizziness, or pain in the arms, jaw, neck, or back. Symptoms can be subtle or mistaken for indigestion or stress, especially in women. If you experience any of these signs, consult a doctor immediately, as early diagnosis can significantly reduce the risk of a heart attack or other complications.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

