7 Shocking Causes of Black Blood You Must Know
What is Black Blood?
Black blood, in a medical and biological context, typically refers to blood that appears dark in color, deviating from the usual bright red hue associated with oxygen-rich arterial blood. This color variation can be attributed to several physiological and pathological conditions that influence the composition and characteristics of blood. Normal blood is red due to the presence of hemoglobin, a protein that binds to oxygen and gives arterial blood its bright red color while deoxygenated blood, returning to the heart, often appears darker. However, under certain circumstances, blood can display shades that may range from dark red to a near-black appearance.
One of the primary reasons for the appearance of black blood is the presence of deoxygenated blood in larger volumes. Conditions such as carbon monoxide poisoning can lead to the formation of carboxyhemoglobin, a compound that has a darker hue. Similarly, situations involving severe anemia or metabolic dysfunctions may result in a higher concentration of reduced hemoglobin, contributing to the dark coloration of the blood. Additionally, some medical conditions, particularly those affecting liver function, such as cirrhosis, can lead to an accumulation of certain metabolites in the bloodstream, causing a blackened appearance.
Moreover, in clinical scenarios like venous blood draws, black blood may be observed when blood clots or if it has been subject to significant decomposition. While the term “black blood” might evoke vivid imagery, it’s essential to note that its occurrence is relatively rare and often signals an underlying health issue that merits medical investigation. Understanding the complexities of blood’s composition and the factors leading to variations is crucial for healthcare professionals in diagnosing and managing health conditions associated with such abnormalities.
The Composition of Blood
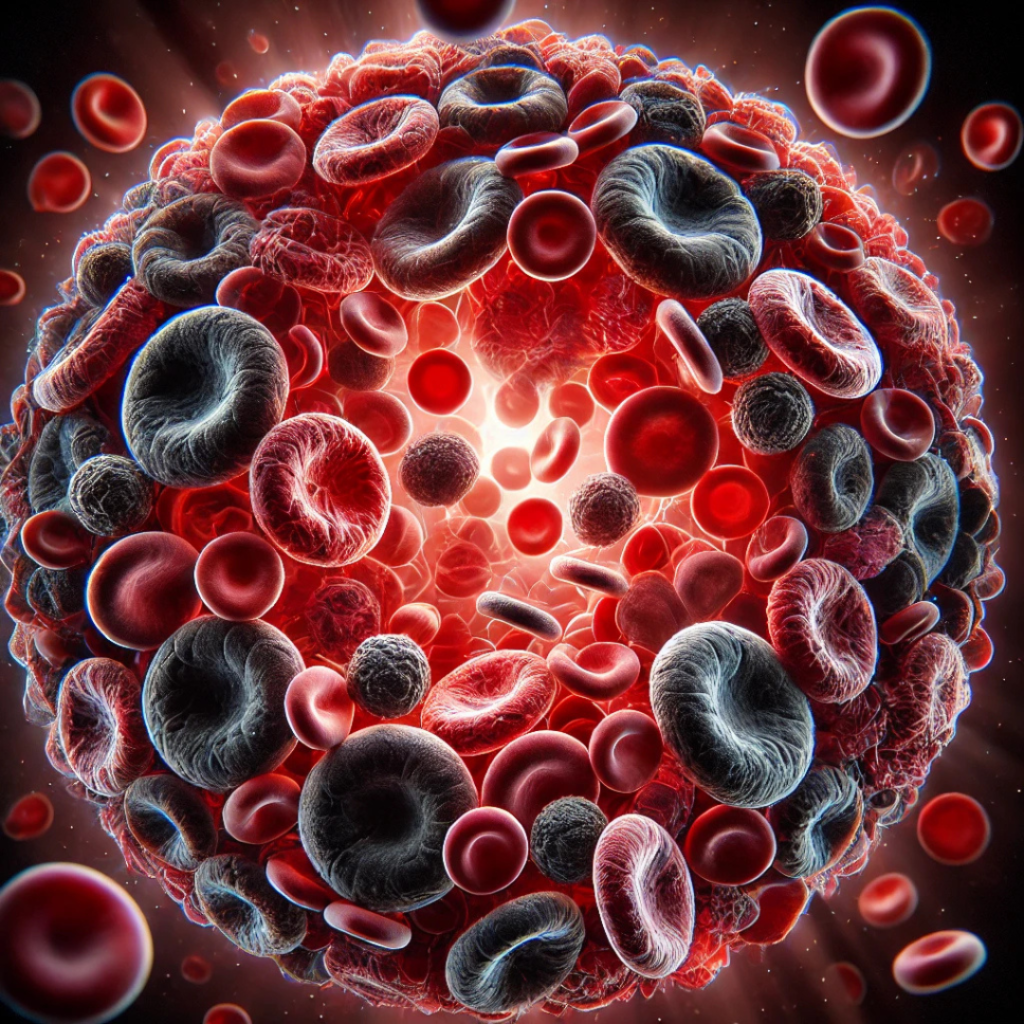
Blood is a vital fluid that plays several critical roles in the human body, primarily transporting nutrients, oxygen, and waste products. The primary components of blood include red blood cells, white blood cells, platelets, and plasma, each with specific functions essential for maintaining health.
Red blood cells (RBCs), or erythrocytes, are the most abundant cells in the bloodstream. Their primary function is to transport oxygen from the lungs to the body’s tissues and return carbon dioxide from the tissues to the lungs for exhalation. Hemoglobin, the protein within RBCs, binds to oxygen and gives blood its red color. The oxidation state of hemoglobin influences blood color; oxygenated blood appears bright red, while deoxygenated blood has a darker red hue. Anomalies in oxygenation can sometimes lead to a blue or purplish tint, which is often misconstrued as black blood.
White blood cells (leukocytes) are essential for the immune response, protecting the body against infections and foreign invaders. They constitute a small fraction of blood volume but are crucial for maintaining health. The various types of white blood cells, including lymphocytes, neutrophils, and monocytes, serve different functions such as antibody production, phagocytosis, and inflammation response.
Platelets, or thrombocytes, are cell fragments involved in blood clotting. They play a significant role in repairing damaged blood vessels and preventing excessive bleeding. When an injury occurs, platelets aggregate at the site and initiate the clotting process, which is vital for wound healing.
Lastly, plasma, the liquid portion of blood, makes up approximately 55% of blood volume. It consists mainly of water, electrolytes, proteins, and various nutrients, serving as a transport medium for cells and solutes. The color of plasma can be influenced by various factors, including hydration levels, diet, and the presence of toxins, which can also affect the overall appearance of blood.
Causes of Dark-Colored Blood
Dark-colored blood can be a surprising and concerning observation for many. Understanding the various medical conditions and external factors responsible for this appearance is essential for accurately assessing one’s health. One significant cause is methemoglobinemia, a condition wherein hemoglobin is altered such that it cannot effectively carry oxygen. This can result from genetic mutations or exposure to certain chemicals, leading to a bluish or darkening of the blood. Scientific studies have demonstrated that methemoglobinemia may occur in both congenital cases and as an acquired condition, with exposure to substances such as nitrates and certain drugs playing pivotal roles.
Another primary contributor to dark blood is infections. Certain severe infections can result in the presence of dark-colored blood due to the effects the pathogens have on the body’s oxygen transportation capabilities. For instance, septicemia can cause a depletion of red blood cells or an alteration in their functionality, leading to darker shades of blood as the body struggles to maintain adequate oxygenation. Research indicates that prompt diagnosis and treatment are vital in preventing the exacerbation of these conditions.
Moreover, hemolytic anemia, a disorder characterized by the premature destruction of red blood cells, can also result in darker blood. In hemolytic anemia, the breakdown of these cells can lead to the release of bilirubin, which may cause blood to appear darker. Factors contributing to this disorder can be varied, including autoimmune diseases and certain infections, according to scientific literature.
Additionally, lifestyle factors such as dehydration can significantly influence blood color. Insufficient fluid intake may result in concentrated blood, which can appear darker. Dietary elements, particularly a lack of iron and certain vitamins, may also impact blood health. Each of these causes highlights the intricate relationship between health and blood characteristics, warranting further investigation for anyone experiencing this phenomenon.

Diagnosing the Issue of Black Blood
Black blood is a condition that prompts immediate medical attention, as it could signify serious underlying health issues. Healthcare professionals utilize a variety of diagnostic procedures and tests to identify the causes of this unusual symptom. Initially, the diagnostic process begins with a detailed medical history, which allows the healthcare provider to understand the patient’s symptoms comprehensively. This step is crucial, as it provides context that informs subsequent tests and evaluations.
Blood tests are a primary tool in diagnosing the causes of black blood. These tests can reveal a range of abnormalities, including altered hemoglobin levels. Hemoglobin is the protein in red blood cells responsible for transporting oxygen; any deviations might indicate health issues such as methemoglobinemia, a condition wherein hemoglobin is altered to a form that cannot effectively carry oxygen, leading to discoloration. Additionally, blood chemistry panels assess renal function and electrolyte levels, which may also play a role in blood anomalies.
Imaging techniques, such as ultrasound or computed tomography (CT) scans, may be employed to visualize internal structures. These can help identify blockages or unusual formations in the cardiovascular system, which could contribute to abnormal blood appearances. For instance, conditions like venous thrombosis may lead to black or darkened blood due to inadequate blood flow.
Through these diagnostic measures, doctors can correlate the findings from clinal examination, blood tests, and imaging studies. Each result helps to piece together the potential causes of black blood, allowing healthcare professionals to develop an appropriate treatment plan. Hence, making the diagnosis of black blood a multifaceted process, requiring a combination of thorough history-taking and systematic testing to ascertain the underlying health condition accurately.
Health Implications of Black Blood
The presence of black blood, while often alarming, can indicate various underlying medical conditions that warrant immediate attention. Black blood is typically a sign of altered hemoglobin, which can occur due to the presence of certain chemicals, a decrease in oxygen, or specific health ailments. One common cause is the production of methemoglobin, a form of hemoglobin that cannot effectively carry oxygen, leading to potential health risks.
Conditions such as carbon monoxide poisoning can also result in blood appearing darker than usual, as the hemoglobin binds more tightly to carbon monoxide than to oxygen. Similarly, certain medical conditions such as liver disease or sepsis may alter blood composition, thus leading to the black coloration. Individuals exhibiting such symptoms should seek medical assistance promptly, as these conditions can escalate rapidly, resulting in severe health consequences.
Moreover, black blood can sometimes suggest a serious vascular or circulatory issue. For example, venous thrombosis can create blockages that might change the appearance of blood returning to the heart. In cases of severe dehydration, the blood may thicken and appear darker. Such conditions can pose significant risks, as they may progress to more severe health complications, including organ failure.
It is critical for individuals who notice the occurrence of black blood, or other related symptoms such as shortness of breath or disorientation, to contact a healthcare provider immediately. Timely diagnosis and intervention are essential for the management of these potentially life-threatening conditions. Understanding that black blood is often a symptom stemming from underlying issues can promote better health awareness and encourage necessary preventative measures for those affected.
Treatment Options for Dark Blood Conditions
Dark blood, medically referred to as black blood, can arise from various underlying conditions, necessitating tailored treatment approaches. The specific treatment options largely depend on the cause of the dark coloration observed in the blood. For instance, if the condition is linked to dietary deficiencies, such as a lack of essential vitamins like B12, dietary modifications can be a primary intervention. Incorporating rich sources of nutrients and appropriate supplements can significantly improve blood health and correct abnormalities.
In cases where dark blood is attributed to hematological disorders, healthcare professionals might recommend medication adjustments. Anticoagulants or antiplatelet therapies, for instance, are critical in managing blood clotting issues. This adjustment helps enhance blood flow and oxygen transport and can alleviate symptoms related to dark blood conditions. Moreover, routine monitoring of patients on such medications is vital to mitigate potential side effects.
Additionally, for those suffering from chronic conditions that contribute to black blood, such as liver disease or respiratory issues, addressing the underlying medical issue becomes imperative. This could involve pharmacological treatments aimed at improving organ function and overall blood oxygenation. For example, treating liver disease may improve the body’s ability to properly filter and regulate blood, leading to healthier coloration.
In emergency situations, if dark blood indicates a critical health issue such as internal bleeding or severe infection, rapid interventions are essential. This may include blood transfusions or hospitalization, ensuring that the patient receives prompt medical attention. Overall, a comprehensive understanding of the cause is foundational in determining the most effective treatment avenues for black blood conditions, promoting recovery and optimizing health outcomes.

Prevention Strategies and Lifestyle Changes
Maintaining healthy blood color and overall blood health is essential for optimal physiological function. Preventive measures and lifestyle adaptations play a crucial role in achieving this goal. One of the primary strategies involves ensuring adequate hydration. Water is vital in maintaining blood viscosity and volume, which can help prevent issues related to blood quality. Aim for at least eight 8-ounce glasses of water daily, adjusting intake based on activity levels and environmental conditions.
A balanced diet is equally significant in promoting healthy blood. Incorporating various foods rich in essential nutrients may improve blood composition. Key components include iron-rich foods like legumes, lean meats, spinach, and fortified cereals, which are vital for hemoglobin production. Additionally, consuming foods high in vitamin C, such as citrus fruits and leafy greens, can enhance iron absorption. A diet that includes omega-3 fatty acids, found in fish, flaxseeds, and walnuts, can also support cardiovascular health and prevent blood clots.
Regular medical check-ups are another indispensable component of blood health management. Routine screenings help detect potential issues early, allowing for timely intervention. Blood tests can provide valuable information about hemoglobin levels and other parameters that establish the overall health of an individual’s blood. Monitoring for signs of anemia or clotting disorders can be crucial in maintaining optimal blood quality.
Additionally, lifestyle choices, such as avoiding smoking and excessive alcohol consumption, can aid in reducing risk factors associated with blood conditions. Engaging in regular physical activity promotes healthy circulation and overall cardiovascular health. Simple activities like walking, cycling, or yoga can significantly benefit your blood. By adopting these preventive measures and lifestyle changes, individuals can effectively manage their blood health and reduce the risk of blood-related issues.
Frequently Asked Questions (FAQs)
Understanding the phenomenon of black blood often raises numerous questions among the public, driven mainly by misconceptions and myths. Here, we address some of the most common inquiries regarding the appearance, causes, and health implications related to black blood.
What does black blood signify?
Black blood typically refers to a darkened hue of blood observed in certain medical conditions. The most common scenario is in cases of severe oxygen deprivation or high levels of deoxyhemoglobin, which can occur in conditions such as methemoglobinemia. In this instance, the blood takes on a dark brownish color, sometimes perceived as black.
Is black blood a sign of serious illness?
The appearance of black blood can indeed be associated with serious medical conditions, but it is essential to understand that not all instances are indicative of a life-threatening issue. Conditions such as specific poisoning or certain blood disorders may result in the dark coloration of blood. However, factors like dehydration can also lead to concentrated blood, altering its appearance. A medical evaluation is crucial for accurate diagnosis.
Can black blood be harmful?
The presence of black blood often signals an underlying problem that may require immediate medical attention, especially if accompanied by other symptoms such as chest pain or difficulty breathing. While black blood in isolation might not be hazardous, it typically reveals a state of hypoxia or inadequate circulation, which can pose risks if left unaddressed. Strategies for management vary based on the root cause of the discoloration.
Does black blood occur in everyone?
No, black blood does not occur in everyone. Its presence typically relates to specific physiological or pathological conditions that disrupt the normal red hue of oxygenated blood. Understanding the reasons behind this extraordinary coloration is essential for anyone concerned about its occurrence.
In conclusion, black blood can be alarming, but scientific knowledge illuminates its causes and health implications. Addressing concerns with a healthcare provider is crucial for proper assessment and intervention.
Conclusion
Understanding blood health is crucial for maintaining overall well-being. The color of blood can serve as an important indicator of various physiological conditions, highlighting the potential for underlying health issues. Throughout this blog post, we have explored the relation between blood color, particularly the phenomenon of black blood, and the insights it provides regarding our health. It is essential to recognize that changes in blood color, whether it is a shift towards a darker hue or other noticeable variations, may suggest significant medical conditions that warrant investigation.
For instance, black blood can be an indication of issues such as carbon monoxide poisoning, certain types of infections, or severe liver dysfunction. By being aware of these possible implications, individuals can take proactive steps in monitoring their health and seeking appropriate medical care when necessary. This understanding emphasizes the importance of listening to one’s body and remaining vigilant about symptoms that arise.
Furthermore, promoting awareness about blood health extends beyond individual observation to encompass broader societal implications. Educational efforts aimed at increasing knowledge about the significance of blood characteristics can empower individuals to engage more actively in health management. Thus, it is vital for readers to remain informed about their own blood health and to consult healthcare professionals in the presence of any concerning symptoms.
In conclusion, the significance of understanding blood health cannot be overstated. Recognizing changes in blood color is not merely a matter of curiosity; it can be a pivotal factor in early detection and intervention of health issues. By maintaining vigilance and seeking timely medical advice, individuals can contribute to their health management and well-being.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

