The Endocrine System
The endocrine system is a sophisticated network of glands that play a crucial role in maintaining homeostasis within the human body. Unlike other systems that might seem more visibly integral to everyday functions, the endocrine system operates behind the scenes, producing and releasing hormones that regulate a variety of bodily functions. These hormones act as chemical messengers, traveling through the blood to tissues and organs and influencing essential processes such as metabolism, growth, and reproduction.
An integral aspect of understanding the endocrine system involves distinguishing between endocrine and exocrine glands. Endocrine glands, which include the thyroid gland, adrenal glands, pituitary gland, and others, release hormones directly into the bloodstream. This direct release mechanism allows hormones to reach target organs or tissues far from their site of origin. In contrast, exocrine glands, such as sweat glands and salivary glands, secrete their products into ducts that lead either to body surfaces or cavities. For instance, sweat glands produce sweat that is excreted through pores in the skin, while salivary glands release saliva into the mouth.
The functions controlled by the endocrine system are diverse and vital. Hormones regulate metabolism by controlling the rate at which the body converts food into energy. They also influence growth by managing the development and differentiation of cells and tissues. Reproductive processes, including the menstrual cycle and sperm production, are also governed by hormonal signals. Additionally, the endocrine system is pivotal in controlling various other physiological activities such as mood regulation, immune response, and maintaining electrolyte balance.
In summary, the endocrine system’s intricate network of glands and hormones is fundamental to the regulation and integration of multiple bodily functions. Understanding this system provides a foundation for appreciating how the body maintains equilibrium and responds to internal and external changes.
Major Endocrine Glands and Their Functions
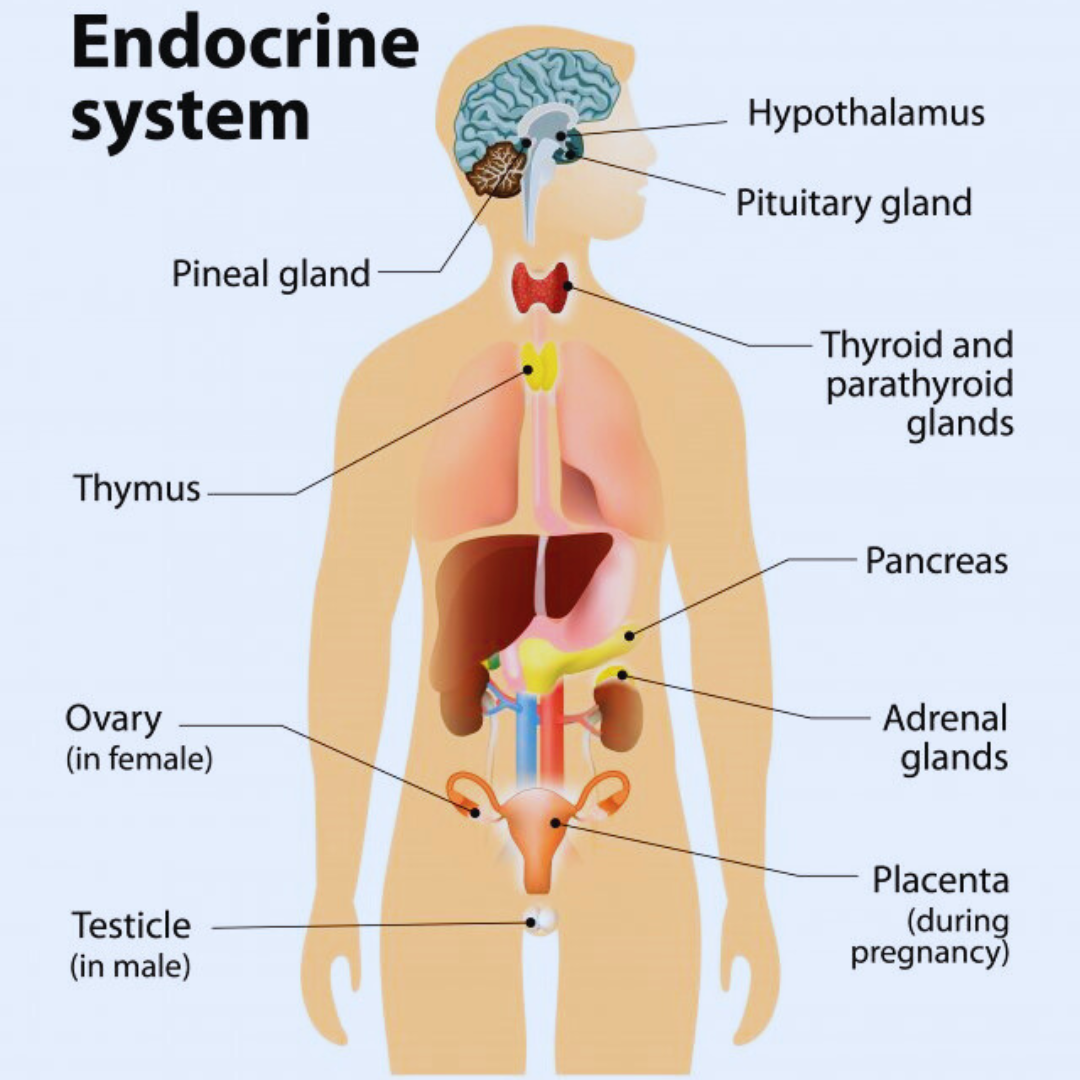
The endocrine system is an intricate network of glands that produce and secrete hormones directly into the bloodstream, regulating numerous bodily functions. Key players in this system include the hypothalamus, pituitary gland, thyroid gland, adrenal glands, pancreas, and gonads. Each of these glands has specific roles and produces essential hormones that maintain homeostasis and facilitate growth and development.
Hypothalamus
Located in the brain, the hypothalamus plays a crucial role in maintaining homeostasis by regulating the autonomic nervous system and orchestrating the activity of various endocrine glands. It produces hormones such as thyrotropin-releasing hormone (TRH) and corticotropin-releasing hormone (CRH), which stimulate the pituitary gland, thereby controlling the release of other hormones throughout the body.
Pituitary Gland
Often termed the “master gland,” the pituitary gland is a pea-sized structure connected to the hypothalamus. It houses two lobes: the anterior and posterior pituitary. The anterior lobe secretes hormones like growth hormone (GH), prolactin, and adrenocorticotropic hormone (ACTH). These hormones influence growth, lactation, and stress response. The posterior lobe releases oxytocin and vasopressin (antidiuretic hormone, ADH), which are vital for childbirth, lactation, and water balance.
Thyroid Gland
The thyroid gland, located in the neck, produces thyroid hormones (T3 and T4) and calcitonin. T3 and T4 are instrumental in regulating metabolism, energy generation, and growth. Calcitonin plays a minor role in calcium homeostasis by inhibiting bone resorption.
Adrenal Glands
Sitting atop each kidney, the adrenal glands are composed of the adrenal cortex and medulla. The cortex produces corticosteroids, such as cortisol, aldosterone, and androgens. Cortisol regulates metabolism and stress responses, while aldosterone manages blood pressure by controlling sodium and potassium levels. The adrenal medulla secretes catecholamines (epinephrine and norepinephrine) during stress, amplifying the body’s fight-or-flight response.
Pancreas
The pancreas has dual functions as both an endocrine and exocrine gland. Its endocrine role involves the secretion of insulin and glucagon by the islets of Langerhans. Insulin lowers blood glucose levels by facilitating cellular uptake, while glucagon increases blood glucose by promoting glycogen breakdown in the liver, ensuring glucose homeostasis.
Gonads
The gonads, comprising the testes in males and ovaries in females, produce sex hormones crucial for reproduction and secondary sexual characteristics. Testes secrete testosterone, which influences sperm production and male physical traits. Ovaries produce estrogen and progesterone, essential for the menstrual cycle, pregnancy, and female secondary sexual characteristics.
The harmonious interplay of these endocrine glands ensures the seamless operation of bodily processes, emphasizing the complexity and importance of the endocrine system in maintaining health and vitality.
Hormones: The Messengers of the Endocrine System
Hormones are pivotal chemical messengers that play integral roles within the endocrine system. Produced by various glands, these substances travel through the bloodstream to specific target organs and tissues, orchestrating a myriad of physiological functions. By binding to unique receptors on or within their target cells, hormones initiate precise, finely-tuned biological responses that regulate everything from growth and metabolism to mood and reproductive processes.
There are several types of hormones, each with distinct characteristics and mechanisms of action. Steroid hormones, such as cortisol and estrogen, are derived from cholesterol and are lipid-soluble. Their solubility allows them to easily diffuse through cell membranes and bind to intracellular receptors, often directly influencing gene expression and protein synthesis within the nucleus.
Peptide hormones, including insulin and growth hormone, are composed of amino acids and are generally water-soluble. They bind to receptors on the cell surface, triggering signaling cascades that result in rapid cellular responses. Unlike steroid hormones, peptide hormones often utilize second messenger systems to amplify their signals inside the target cells.
Hormones also vary in their transportation through the circulatory system. Some, like thyroid hormones, are bound to carrier proteins, which protect them from degradation and extend their half-life. Others circulate freely and interact with their target cells more directly. The specificity of hormonal effects is largely determined by the presence of compatible receptors on target cells, ensuring that only those cells respond to a particular hormone.
Overall, the precision and specificity of hormone interactions underscore their critical role in maintaining homeostasis. The intricate network of hormone signaling exemplifies the complexity of the endocrine system, highlighting its essential function in synchronizing physiological processes throughout the body.

Regulation of Hormone Levels
The regulation of hormone levels is a crucial aspect of the endocrine system’s function, ensuring that the body maintains homeostatic balance. Hormone levels are primarily regulated through complex mechanisms involving feedback loops, which can be categorized into negative feedback and positive feedback loops.
Negative feedback loops are the most common mechanism for maintaining hormone balance. In this system, an increase in the level of a specific hormone will trigger a response that decreases its production. For example, the endocrine system regulates blood sugar levels via insulin and glucagon. When blood sugar levels rise, the pancreas secretes insulin, promoting the uptake of glucose by cells and thereby reducing blood glucose levels. Conversely, when blood glucose levels drop, glucagon is released to promote the conversion of glycogen to glucose, elevating blood sugar levels.
Positive feedback loops, while less common, amplify the initial stimulus. One prominent example is the release of oxytocin during childbirth. The stretching of the cervix triggers the release of oxytocin, which stimulates uterine contractions. These contractions, in turn, cause further stretching of the cervix, leading to more oxytocin release until delivery occurs.
Central to the regulation of hormone levels is the role of the hypothalamus and the pituitary gland. These two structures act as the command center for endocrine regulation. The hypothalamus receives signals from various parts of the body and the environment, responding by releasing hormones that control the pituitary gland’s activity. The pituitary gland, often referred to as the “master gland,” secretes hormones that influence other endocrine glands, including the thyroid, adrenal glands, and gonads, to release their respective hormones.
An example of this regulation is how the body maintains calcium homeostasis. The parathyroid glands, in response to low blood calcium levels, secrete parathyroid hormone (PTH) which increases calcium levels by stimulating the release of calcium from bones, increasing calcium absorption in the intestines, and promoting calcium reabsorption in the kidneys. When calcium levels rise, the production of PTH is inhibited, exemplifying a negative feedback loop.
Through these feedback mechanisms, the endocrine system ensures that hormone levels are meticulously controlled, allowing the body to adjust to internal and external changes effectively.
Common Endocrine Disorders
The endocrine system plays a pivotal role in regulating the body’s hormones, which in turn influence numerous bodily functions. When this system encounters disruptions, it can lead to various endocrine disorders, each with distinct symptoms, causes, and treatments. Prominent among these disorders are diabetes mellitus, hypothyroidism, hyperthyroidism, Addison’s disease, and polycystic ovary syndrome (PCOS). Recognizing and managing these disorders early is crucial to prevent severe complications.
Diabetes mellitus is a chronic condition characterized by high blood sugar levels due to insulin deficiency or resistance. Symptoms include excessive thirst, frequent urination, and unexplained weight loss. This disorder is typically managed through lifestyle modifications, oral medications, and in some cases, insulin therapy. Ensuring tight blood sugar control is essential to minimize risks of complications such as neuropathy, nephropathy, and cardiovascular diseases.
Hypothyroidism occurs when the thyroid gland produces insufficient thyroid hormone, leading to symptoms like fatigue, weight gain, and cold intolerance. Causes can range from autoimmune diseases (like Hashimoto’s thyroiditis) to iodine deficiency. Treatment usually involves daily administration of synthetic thyroid hormone to normalize hormone levels.
Conversely, hyperthyroidism is characterized by excessive thyroid hormone production, which can cause weight loss, rapid heartbeat, and anxiety. Graves’ disease is a common cause. Treatment options include antithyroid medications, radioactive iodine therapy, or sometimes surgery to remove part of the thyroid gland.
Addison’s disease, also known as primary adrenal insufficiency, results from adrenal gland damage leading to insufficient production of cortisol and aldosterone. Symptoms often include chronic fatigue, muscle weakness, and low blood pressure. Lifelong hormone replacement therapy is necessary to manage this condition effectively.
Polycystic ovary syndrome (PCOS) is a prevalent endocrine disorder among women of reproductive age, marked by irregular menstrual periods, excess androgen levels, and polycystic ovaries. Treatments are tailored to manage symptoms and may include hormonal contraceptives to regulate menstrual cycles, medications to manage insulin resistance, and lifestyle changes.
These disorders highlight the importance of early diagnosis and appropriate management to maintain optimal health. Regular check-ups and patient education can empower individuals to recognize symptoms early and seek timely medical intervention.
The Impact of Lifestyle on Endocrine Health
The endocrine system, an ensemble of glands and organs where hormones are synthesized, plays a pivotal role in regulating various bodily functions. It’s increasingly apparent that lifestyle factors such as diet, exercise, stress, and sleep significantly influence endocrine health. By adopting healthy habits, one can enhance hormone production and balance, while unfavorable choices can lead to disruption and disorders.
Diet is integral to maintaining endocrine balance. Consuming a diet rich in whole foods, fruits, vegetables, lean proteins, and healthy fats supports hormone production. Foods high in omega-3 fatty acids, such as salmon and flaxseeds, are particularly beneficial. Conversely, diets laden with processed foods, excessive sugars, and unhealthy fats can impair hormone function. Monitoring caffeine and alcohol intake is equally crucial, as they can lead to an overstimulated or disrupted endocrine response.
Regular physical activity is another cornerstone of endocrine health. Exercise aids in regulating the release of endorphins and other hormones, thus promoting overall hormonal balance. It contributes to weight management, positively influencing hormones like insulin and cortisol. Incorporating a combination of cardiovascular, strength training, and flexibility exercises can yield the best outcomes.
Stress management is equally essential in maintaining a healthy endocrine system. Chronic stress triggers the release of cortisol, the body’s primary stress hormone, disrupting other hormonal functions over time. Techniques such as mindfulness, meditation, yoga, and breathing exercises are effective in alleviating stress. Seeking professional help for chronic stress or anxiety disorders can also be beneficial.
Adequate sleep is imperative for endocrine health. Quality sleep enables the release of growth hormones and the proper functioning of other crucial hormones. Adults should aim for 7-9 hours of sleep per night, emphasizing a consistent sleep schedule and a restful sleep environment. Avoiding screens before bedtime and establishing a wind-down routine can further improve sleep quality.
Practical steps for maintaining a healthy endocrine system through lifestyle modifications include eating nutrient-dense meals, engaging in regular exercise, managing stress effectively, and ensuring sufficient sleep. Prioritizing these aspects of lifestyle can greatly enhance endocrine health, fostering overall well-being.

Recent Advances in Endocrinology
The field of endocrinology has undergone significant advancements in recent years, leading to improved diagnostic tools, treatments, and a deeper understanding of various endocrine disorders. One of the pivotal developments is the advent of precision medicine, which has revolutionized the way endocrinologists diagnose and treat conditions. By utilizing genetic profiling, medical professionals can tailor treatments to an individual’s unique genetic makeup, resulting in more effective and personalized patient care.
In diagnosing endocrine disorders, innovations such as enhanced imaging techniques and biomarker identification have played a critical role. High-resolution ultrasound and MRI have significantly improved the accuracy of diagnosing thyroid nodules and adrenal tumors. Additionally, the utilization of liquid biopsy, a non-invasive technique analyzing circulating tumor DNA, shows promising potential for early detection of endocrine cancers.
On the treatment frontier, there has been remarkable progress in the development of novel therapies. For instance, the introduction of small molecule inhibitors and monoclonal antibodies has opened new avenues for treating conditions like acromegaly and Cushing’s syndrome. In the context of diabetes management, the approval of SGLT-2 inhibitors and GLP-1 receptor agonists has greatly enhanced glycemic control and cardiovascular outcomes for patients with type 2 diabetes.
Further understanding of endocrine disorders has been bolstered by advances in genomics and epigenetics. Researchers have identified numerous genetic mutations and epigenetic changes linked to conditions such as congenital adrenal hyperplasia and polycystic ovary syndrome. This deeper knowledge facilitates the development of targeted therapies and has the potential to improve long-term patient outcomes.
Looking ahead, the trajectory of endocrinology suggests continued integration of cutting-edge technologies and interdisciplinary collaboration. Areas such as artificial intelligence and machine learning are expected to further refine diagnostic accuracy and treatment personalization. The ongoing improvements in endocrine research and treatment methodologies underscore a promising future for patient care and outcomes, highlighting the dynamic nature of the field.
Endocrine System FAQs
The endocrine system is an intricate network of glands and organs responsible for regulating bodily functions through the secretion of hormones. Below are answers to some frequently asked questions about this vital system.
What are hormones?
Hormones are chemical messengers produced by endocrine glands and released into the bloodstream. They travel to various tissues and organs, influencing diverse processes such as metabolism, growth, and mood. These substances ensure our body operates cohesively by maintaining balance and communication between different physiological systems.
How do endocrine glands communicate?
Endocrine glands communicate through the release and reception of hormones. For instance, the pituitary gland, often referred to as the “master gland,” releases hormones that control other endocrine glands, such as the thyroid and adrenal glands. This communication is vital for adjusting bodily functions in response to internal and external stimuli.
What are the symptoms of hormonal imbalances?
Symptoms of hormonal imbalances can vary widely depending on which hormones are affected. Common signs include fatigue, unexplained weight gain or loss, mood swings, and changes in appetite or sleep patterns. Women may experience irregular menstrual cycles, while men might notice issues with hair growth. Recognizing these symptoms is crucial for timely medical intervention.
Can lifestyle changes improve endocrine health?
Yes, lifestyle changes can significantly enhance endocrine health. Regular physical activity, a balanced diet rich in nutrients, stress management, and adequate sleep play pivotal roles in maintaining hormonal balance. Avoiding excessive consumption of alcohol, caffeine, and sugar can also contribute to a healthier endocrine system. Consulting with healthcare professionals for personalized advice is advised.
What should I do if I suspect an endocrine disorder?
If you suspect an endocrine disorder, schedule an appointment with a healthcare provider. Medical professionals can perform diagnostic tests, evaluate symptoms, and propose suitable treatments. Early detection and management are vital for effectively addressing endocrine disorders and mitigating potential complications.
Which organs are part of the endocrine system?
The endocrine system comprises glands such as the pituitary, thyroid, adrenal, and pineal glands, as well as organs like the pancreas, ovaries, and testes. Each plays a unique role in regulating processes like metabolism, reproduction, and stress response.
How does the thyroid gland affect the body?
The thyroid gland produces hormones that regulate metabolism, energy levels, and body temperature. An overactive thyroid (hyperthyroidism) or underactive thyroid (hypothyroidism) can lead to symptoms like weight changes, fatigue, and mood disturbances.
What role does the pancreas play in endocrine function?
The pancreas has a dual role, functioning as both an endocrine and exocrine organ. Its endocrine role includes producing insulin and glucagon, which regulate blood sugar levels, crucial for energy balance and metabolic health.
What is the difference between type 1 and type 2 diabetes?
Type 1 diabetes is an autoimmune condition where the pancreas produces little or no insulin. Type 2 diabetes, more common, occurs when the body becomes resistant to insulin or the pancreas doesn’t produce enough. Both affect endocrine function and require tailored management.
Can stress impact the endocrine system?
Yes, chronic stress triggers the adrenal glands to release cortisol, the stress hormone. Prolonged elevation of cortisol can disrupt other hormonal balances, potentially affecting metabolism, immune response, and mental health.
Are endocrine disorders hereditary?
Some endocrine disorders, such as type 1 diabetes, hypothyroidism, and polycystic ovary syndrome (PCOS), can have a genetic component. Family history may increase susceptibility, but environmental and lifestyle factors also play a role.
How does aging affect the endocrine system?
As people age, endocrine function may decline. For example, the production of sex hormones like estrogen and testosterone decreases, leading to menopause or andropause. Similarly, growth hormone levels and metabolism tend to slow down with age.
What is the difference between endocrine and exocrine glands?
Endocrine glands release hormones directly into the bloodstream to regulate bodily functions. In contrast, exocrine glands, such as sweat or salivary glands, secrete substances through ducts to the surface of the skin or into body cavities.
Can endocrine disorders be prevented?
While not all endocrine disorders are preventable, maintaining a healthy lifestyle—balanced diet, regular exercise, stress reduction, and adequate sleep—can reduce the risk of developing conditions like type 2 diabetes and thyroid imbalances.
Why is the pituitary gland called the “master gland”?
The pituitary gland controls several other endocrine glands by releasing hormones that influence their activity. It regulates vital functions such as growth, reproduction, and metabolism, making it central to endocrine system coordination.
What is the role of the adrenal glands?
The adrenal glands produce hormones like adrenaline, cortisol, and aldosterone, which help the body respond to stress, regulate blood pressure, and maintain electrolyte balance.
How does the endocrine system interact with other systems?
The endocrine system works closely with the nervous and immune systems to maintain homeostasis. For example, it influences the nervous system through stress hormones and supports immune responses by regulating inflammation.
Understanding the fundamental aspects of the endocrine system and addressing common concerns can empower individuals to take proactive steps towards maintaining hormonal health. Regular check-ups and open communication with healthcare providers are essential for optimal endocrine function.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

