White Blood Cells (Leukocytes): 5 Unique Benefits
Understanding White Blood Cells
White blood cells, or leukocytes, play a pivotal role in the immune system, serving as the body’s primary defense mechanism against infections and foreign invaders. These specialized cells are an essential component of the immune response, working diligently to detect, target, and eliminate pathogens such as bacteria, viruses, and fungi. Understanding white blood cells is crucial for comprehending how our body maintains health and fights disease.
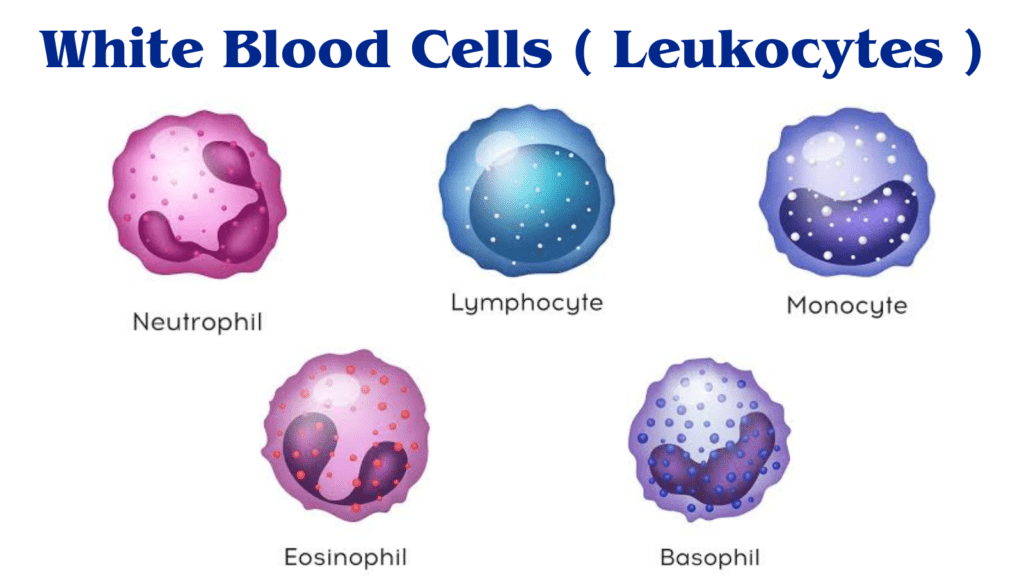
There are several distinct types of white blood cells, each with unique functions and characteristics. The major categories include lymphocytes, neutrophils, monocytes, eosinophils, and basophils. Lymphocytes, which include T cells and B cells, are instrumental in recognizing and remembering specific pathogens, allowing for a faster response upon re-exposure. Neutrophils are often the first responders to sites of infection, rapidly engulfing and destroying bacteria. Monocytes, upon migrating to tissues, transform into macrophages that further cleanse the area of pathogens and dead cells. Eosinophils and basophils play roles in the body’s response to allergies and parasitic infections, further illustrating the diverse roles white blood cells fulfill in immune defense.
The functionality of white blood cells is governed by a complex interplay of signaling mechanisms, whereby they communicate with one another to effectively mount an immune response. For instance, when a pathogen breaches the body’s defenses, various white blood cells are summoned to the site of infection through chemical signals known as cytokines. This coordinated effort allows for the rapid neutralization and clearance of invaders, maintaining homeostasis and health. In summary, white blood cells are not merely defenders but are integral to the overall functioning and resilience of the immune system, ensuring the body can effectively combat a wide array of health threats.
The Different Types of White Blood Cells
White blood cells, or leukocytes, play a crucial role in the immune system by defending the body against infections and foreign substances. There are several distinct types of white blood cells, each with specialized functions that contribute to the overall immune response. The five primary types include neutrophils, lymphocytes, monocytes, eosinophils, and basophils, each playing a vital role in maintaining the body’s health.
Neutrophils are the most abundant type of white blood cell, accounting for approximately 55-70% of the total leukocyte count. These cells are the first responders to sites of infection or tissue injury, effectively engulfing and destroying bacteria and fungi through a process called phagocytosis. They have a short lifespan, typically lasting only a few days, yet their rapid response is essential in combating acute infections.
Lymphocytes are another critical component of the immune system, with three primary subtypes: B cells, T cells, and Natural Killer (NK) cells. B cells are responsible for producing antibodies, which target and neutralize pathogens. T cells can be further categorized into helper T cells, which assist other immune cells, and cytotoxic T cells, which directly kill infected cells. NK cells play a vital role in recognizing and destroying compromised host cells, providing innate immunity.
Monocytes, which account for about 2-8% of the white blood cells, are larger than other leukocytes and can differentiate into macrophages and dendritic cells. Macrophages are powerful phagocytes that engulf and digest pathogens and dead cells, while dendritic cells serve as antigen-presenting cells, facilitating the activation of T cells. Eosinophils make up 1-4% of white blood cells and are primarily involved in combating multicellular parasites and mediating allergic reactions. Lastly, basophils, the least common type, release histamine and play a role in inflammatory responses.
Understanding these different types of white blood cells and their unique functions is essential for appreciating how the immune system operates to protect the body from illness and infection.
The Process of White Blood Cell Formation
White blood cells (WBCs), or leukocytes, play a crucial role in the body’s immune response. Their formation takes place primarily in the bone marrow through a process known as hematopoiesis. This intricate procedure involves the differentiation of hematopoietic stem cells, which are multipotent cells capable of developing into various blood cell types, including red blood cells, platelets, and WBCs.
Hematopoiesis begins with the stimulation of hematopoietic stem cells by various cytokines and growth factors such as interleukins and colony-stimulating factors. These signals drive the stem cells down specific lineages, resulting in the development of distinct types of leukocytes. The primary categories include lymphocytes (such as T cells, B cells, and natural killer cells), myeloid cells (which give rise to neutrophils, eosinophils, basophils, and monocytes), and dendritic cells. Each type of WBC has a specialized function, playing a vital role in the defense against pathogens and foreign substances.
The lifespan of white blood cells varies significantly depending on their type. Neutrophils, the most abundant type of WBC, typically have a lifespan of just a few hours to a few days while actively responding to infections. In contrast, memory lymphocytes can persist for years, providing long-term immunity against previously encountered pathogens. Once matured, these cells exit the bone marrow and enter the bloodstream, where they circulate throughout the body, traversing into tissues as needed to perform their functions.
Factors such as infections, inflammatory conditions, and chronic diseases can influence the production and lifespan of WBCs. For example, during an infection, the body may increase the production of specific leukocytes to mount an effective immune response. Overall, the dynamic process of white blood cell formation ensures that the immune system remains adept at identifying and responding to threats in a timely manner.

White Blood Cells in Action: Immune Response Mechanism
White blood cells (WBCs) play a pivotal role in the immune response, acting as the body’s first line of defense against infectious agents such as bacteria, viruses, and fungi. When pathogens invade the body, the immune response is initiated through a series of well-coordinated steps, beginning with the recognition of the foreign invaders. Each distinct type of WBC contributes to this process, ensuring a tailored response to a variety of threats.
The initial phase involves the detection of pathogens by specialized cells known as antigen-presenting cells (APCs), which include macrophages and dendritic cells. These cells identify foreign antigens, which are unique markers found on the surface of pathogens. Once activated, APCs migrate to lymph nodes, where they present the antigens to T lymphocytes (T cells), effectively alerting the immune system to the presence of an infection.
Upon recognition, T cells become activated, proliferating and differentiating into various effector cells. Cytotoxic T cells, for example, specifically target and destroy infected cells, while helper T cells release signaling molecules that enhance the activity of other immune cells, including B lymphocytes (B cells) and macrophages. B cells, upon activation, produce antibodies that bind to antigens, neutralizing pathogens and marking them for destruction by other immune cells.
This intricate coordination ensures a robust immune response. In addition to T and B cells, other WBCs such as natural killer (NK) cells and granulocytes also participate in the elimination of pathogens. NK cells are crucial in recognizing and killing infected cells, while granulocytes, including neutrophils and eosinophils, work to engulf and digest foreign invaders. Through these collaborative efforts, the immune system effectively clears infections and restores health to the body.
Common Disorders Related to White Blood Cells
White blood cells (WBCs), or leukocytes, play a critical role in our immune system, serving as the body’s primary defense against infections and diseases. However, when the balance and functionality of these cells are disrupted, various disorders may arise, significantly impacting an individual’s health. Notable conditions associated with white blood cells include leukopenia, leukocytosis, and leukemia, each with distinct symptoms and underlying causes.
Leukopenia refers to a decrease in the number of white blood cells in the bloodstream, typically defined as having fewer than 4,000 WBCs per microliter. This condition can result from factors such as bone marrow dysfunction, autoimmune diseases, or the effects of radiation or chemotherapy. Individuals with leukopenia are more susceptible to infections, as the reduced leukocyte count impairs the body’s ability to combat pathogens. Symptoms may not always be apparent initially, but when infections occur, they can manifest as fever, chills, or persistent fatigue.
In contrast, leukocytosis is characterized by an unusually high count of white blood cells, generally exceeding 11,000 WBCs per microliter. This elevation can result from various causes, including infections, inflammation, stress, or more serious conditions such as leukemia. Symptoms associated with leukocytosis may include fever, malaise, and night sweats, although the condition might sometimes remain asymptomatic. Understanding the underlying cause of leukocytosis is pivotal for determining appropriate treatment strategies.
Leukemia, on the other hand, is a cancer of the blood-forming tissues, primarily the bone marrow. This disorder leads to the production of abnormal white blood cells, which do not function effectively. Symptoms of leukemia can be quite severe and may include weakness, recurrent infections, and easy bruising or bleeding. The prognosis and treatment of leukemia can vary widely depending on its type, such as acute lymphoblastic leukemia or chronic myeloid leukemia, necessitating comprehensive medical evaluation for proper management.
The Role of White Blood Cells in Chronic Diseases
White blood cells (WBCs) play a crucial role in the human immune system, primarily serving to defend against pathogens and maintain homeostasis. However, in certain scenarios, these immune cells can become a contributing factor to chronic diseases. Autoimmune disorders, allergies, and some cancers exemplify situations where WBCs may act in detrimental ways, inadvertently exacerbating health issues rather than alleviating them.
In autoimmune disorders, for instance, the body mistakenly identifies its own tissues as foreign invaders. This leads to an inappropriate activation of white blood cells, which attack healthy cells, resulting in inflammation and damage. Diseases such as rheumatoid arthritis and lupus illustrate how this misguided response can lead to chronic pain, tissue destruction, and significant morbidity.
Allergies represent another instance where WBCs misbehave. In allergic reactions, the immune system overreacts to typically harmless substances, such as pollen or pet dander. This hyper-activation leads to an increased production of immunoglobulin E (IgE) antibodies, which signal white blood cells to release histamines and other inflammatory mediators. This immune response results in symptoms ranging from mild irritation to severe anaphylactic shock, showcasing how WBCs can contribute to chronic conditions.
Certain cancers further illustrate the double-edged sword of white blood cells’ involvement in health. Tumors can exploit immune responses, creating an environment that allows cancer cells to evade immune detection, while some types of WBCs may promote tumor growth. Moreover, chronic inflammation, often driven by white blood cells, is a well-established factor in the progression of various malignancies, highlighting the complex relationship between WBCs and chronic diseases.
Understanding how white blood cells function in these contexts opens up avenues for targeted therapies that aim to modulate immune responses and mitigate the adverse effects of these cells in chronic disease management.

Advancements in White Blood Cell Research
Recent years have witnessed significant advancements in the field of white blood cell research, particularly in the realms of immunotherapy and novel treatment approaches. White blood cells, or leukocytes, play an essential role in the immune system, and understanding their function has become increasingly critical in developing effective therapeutic strategies against various diseases, including cancers and autoimmune disorders.
One notable breakthrough is the adoption of CAR-T cell therapy, a form of immunotherapy that involves the genetic modification of a patient’s own T cells. This technique enhances the ability of these white blood cells to recognize and destroy cancer cells. CAR-T therapies have shown remarkable success in treating certain hematologic malignancies, sparking great interest in similar approaches aimed at solid tumors. Researchers are now focusing on optimizing CAR-T cells to improve their persistence and efficacy in fighting different cancer types.
Additionally, advancements in the understanding of regulatory T cells (Tregs) have opened up new avenues for therapeutic intervention in autoimmune diseases. Tregs are crucial for maintaining immune tolerance, and modifying their activity has the potential to alleviate conditions such as lupus and multiple sclerosis. Researchers have been exploring drug compounds that can selectively enhance Treg function to promote remission in these chronic autoimmune conditions.
Moreover, ongoing studies are investigating the microbiome’s impact on white blood cells, revealing how gut health influences immune responses. The relationship between gut bacteria and immune system function may provide novel therapeutic targets to enhance the efficacy of vaccines and increase protection against infectious diseases.
Looking ahead, the future of white blood cell research appears promising. As new technologies and methodologies emerge, such as single-cell sequencing and machine learning, researchers will be equipped to unravel the complexities of white blood cell dynamics more effectively. This knowledge will not only foster innovative treatment strategies but also offer the potential for personalized medicine, thereby enhancing patient outcomes across various health conditions.
FAQs About White Blood Cells
White blood cells (WBCs), or leukocytes, play a crucial role in our immune system by defending the body against infections and diseases. With their importance in maintaining health, many individuals have questions regarding white blood cells and related health concerns. Here are some frequently asked questions that can enhance the understanding of white blood cells.
How can I boost my white blood cell count?
To enhance white blood cell production, it is essential to adopt a balanced lifestyle that includes a nutritious diet, regular physical activity, and adequate sleep. Consuming foods rich in vitamins and minerals, particularly vitamins C, D, and zinc, can positively influence white blood cell levels. Additionally, managing stress through relaxation techniques such as meditation or yoga can also support a healthy immune response.
What do low white blood cell counts indicate?
A low white blood cell count, a condition known as leukopenia, may signal several underlying health issues. Common causes include autoimmune disorders, certain medications, bone marrow problems, or serious infections. Individuals with low white blood cell counts might experience increased susceptibility to infections and illness. Thus, it is crucial for individuals experiencing low levels to consult with a healthcare professional for appropriate diagnosis and intervention.
Can white blood cells be harmful?
While white blood cells are typically the body’s protectors, there are instances where they can be harmful. For example, when white blood cells mistakenly attack healthy organs or tissues, this can result in autoimmune diseases. Additionally, certain white blood cell types may proliferate abnormally, leading to conditions such as leukemia. Understanding the dual roles of these cells emphasizes the necessity of maintaining a balanced immune response.
How do white blood cells fight infections?
White blood cells are the body’s primary defense against infections. They identify and destroy harmful pathogens such as bacteria, viruses, and fungi. There are different types of white blood cells, each with a unique role. For example, neutrophils quickly respond to bacterial infections by engulfing and destroying bacteria. Lymphocytes, on the other hand, produce antibodies to target and neutralize viruses and other pathogens. This coordinated response is essential in preventing illness and maintaining health.
What happens if you have too many white blood cells?
Having too many white blood cells, a condition known as leukocytosis, can also indicate underlying health problems. It may occur as a response to infection, inflammation, or stress. However, an abnormally high white blood cell count can also be linked to serious conditions such as leukemia or other bone marrow disorders. If someone experiences symptoms like fever, unexplained weight loss, or fatigue, it is important to consult a healthcare professional for evaluation and appropriate treatment.
Overall, maintaining a healthy lifestyle and awareness of these factors can aid in managing white blood cell levels and promoting overall immune system health.
Conclusion
In summary, white blood cells (WBCs) are critical components of the immune system, playing a vital role in protecting the body from infections, diseases, and foreign invaders. These cells, often referred to as leukocytes, encompass various types that work collaboratively to identify, attack, and eliminate pathogens. Each type of white blood cell has a specific function, whether it is the swift response of neutrophils to acute infections, the memory capabilities of lymphocytes that confer long-term immunity, or the regulatory roles of monocytes and eosinophils. Their unique contributions are essential for maintaining health and facilitating recovery from illnesses.
Understanding the functions of white blood cells is paramount, particularly as we navigate advancements in medical research. This ongoing research provides insights into how these cells respond to pathogens, their behavior in the presence of diseases, and the implications of disorders that affect their production and function. For instance, conditions like leukemia, autoimmune diseases, and immunodeficiencies emphasize the need to further study the complexities of WBCs. It is crucial to engage in systematic investigations to unravel the mechanisms by which these cells operate, which may lead to innovative therapeutic strategies and improved treatment options.
As scientific exploration continues, there is hope that we will gain deeper insights into the nuanced roles of white blood cells in not only combating infections but also in the pathology of various diseases. Ultimately, a comprehensive understanding of leukocytes will significantly contribute to enhancing human health outcomes and developing targeted therapeutic interventions. The guardians of our immune system, white blood cells, remain a critical focus of research as we strive to unlock the full potential of our innate defenses against disease.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

