7 Critical Facts About Understanding Angina Today
Understanding Angina
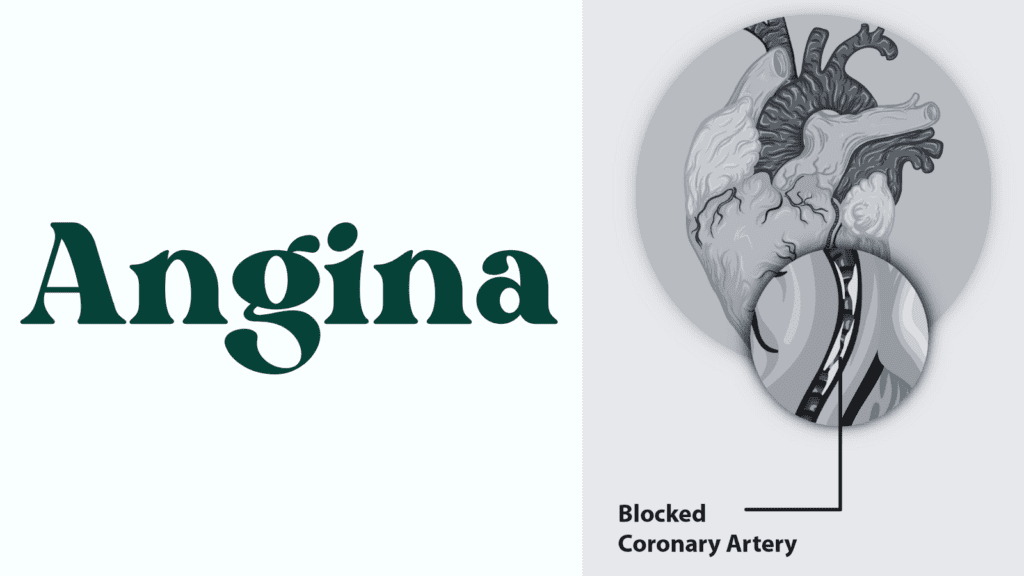
Angina is a clinical term used to describe chest pain or discomfort that arises due to insufficient blood flow and oxygen to the heart muscle. It is important to understand that angina is not a disease in itself but rather a symptom of underlying heart conditions, predominantly coronary artery disease (CAD). This condition occurs when the coronary arteries become narrowed or blocked, often due to atherosclerosis, which is the buildup of fats, cholesterol, and other substances on arterial walls. Angina can manifest in various forms, each having distinct characteristics and triggers.
There are primarily three types of angina: stable, unstable, and variant angina, also known as Prinzmetal’s angina. Stable angina is the most common form and typically occurs during physical exertion or emotional stress. It tends to follow a predictable pattern, with episodes lasting a few minutes and alleviated by rest or medication. Unstable angina, on the other hand, is more serious and occurs unexpectedly, often while at rest. It is characterized by increased frequency and severity of pain and may signal an impending heart attack, necessitating immediate medical attention.
Variant angina, or Prinzmetal’s angina, is a rare type of chest pain that results from temporary spasms in the coronary arteries. These spasms can occur at rest and usually happen during nighttime or early morning hours. While it may not be caused directly by physical exertion, stress or other factors can trigger these episodes. Understanding the differences among these types is crucial for timely diagnosis and management, highlighting the importance of seeking medical advice when experiencing chest pain or discomfort.
Symptoms of Angina
Angina is often characterized by a range of symptoms that primarily revolve around chest pain or discomfort. This chest pain is typically described as a sensation of pressure, squeezing, or fullness that may occur during physical exertion or emotional stress. Individuals experiencing angina may find that the discomfort can radiate to other areas, such as the shoulders, neck, back, arms, or even the jaw. It is crucial to recognize that the intensity and duration of chest pain can vary significantly from person to person.
In addition to the prominent chest pain, individuals may experience accompanying symptoms that are important for diagnosing underlying heart conditions. One common symptom is shortness of breath, which may occur during physical activity or even at rest in some cases. This symptom can signify that the heart is not receiving adequate blood flow, a characteristic associated with angina. It is essential for individuals to pay attention to any episodes of breathlessness, as they can indicate worsening heart health.
Other potential symptoms of angina include nausea, which can often accompany the feeling of chest discomfort, and fatigue, which may arise from the body’s diminished ability to exert itself due to inadequate blood circulation. Some individuals may also report symptoms such as dizziness or an abnormal heartbeat. Recognizing and understanding these symptoms is vital, as they can serve as warning signs of coronary artery disease or other serious heart issues.
If you or someone you know experiences chest pain or any of these symptoms, it is imperative to seek medical attention. Open conversations with healthcare providers regarding these symptoms can lead to timely diagnoses and effective treatment plans, ultimately preventing more severe cardiac events.
Causes and Risk Factors of Angina
Angina, a type of chest pain, is primarily caused by coronary artery disease (CAD), which occurs when the coronary arteries that supply blood to the heart muscle become narrowed or blocked. This narrowing is often due to atherosclerosis, a condition characterized by the buildup of fatty plaques on the artery walls. These plaques limit blood flow, particularly during physical activity or stress, leading to the characteristic symptoms of angina.
Several risk factors significantly contribute to the development of coronary artery disease and, subsequently, angina. Key modifiable risk factors include high cholesterol levels, high blood pressure, and smoking. Elevated cholesterol can result in plaque formation in the arteries, while high blood pressure can damage artery walls and exacerbate plaque buildup. Smoking further compounds these issues, as it not only reduces oxygen availability but also leads to inflammation and injury of the blood vessels.
Diabetes is another critical risk factor, as it can accelerate the process of atherosclerosis and diminish blood flow. Individuals with diabetes often experience higher levels of harmful lipids in their blood, which can further contribute to narrowing arteries. A sedentary lifestyle also plays a notable role; physical inactivity can lead to weight gain and poor cardiovascular health, which increase the likelihood of developing angina.
In addition to these modifiable risk factors, there are non-modifiable factors that individuals should consider. Age is a significant risk factor, as the likelihood of heart-related issues generally increases with advancing age. Furthermore, genetics can also play a role, as a family history of heart disease can predispose individuals to similar conditions. Understanding these causes and risk factors of angina is essential for effective prevention and management strategies.

Diagnosis of Angina
Diagnosing angina is a critical process that healthcare professionals undertake to ensure appropriate treatment plans are established. The evaluation typically begins with a comprehensive medical history and a detailed discussion of the patient’s symptoms. Information about the frequency, duration, and triggers of the chest pain helps clinicians understand the severity and potential causes of angina.
After the initial assessment, a physical examination is conducted to check for risk factors, such as high blood pressure or elevated cholesterol levels. These factors can indicate the presence of coronary artery disease, which is often associated with angina. Once the initial evaluations are complete, various diagnostic tests may be employed to confirm the diagnosis and assess heart function.
One of the most common diagnostic tests for angina is the electrocardiogram (ECG), which measures the electrical activity of the heart. An ECG can reveal irregularities in heart rhythms or signs of reduced blood flow during episodes of angina. Stress tests are frequently conducted as well, where the patient exercises on a treadmill or stationary bike while heart activity is monitored. This test evaluates how well the heart responds to physical exertion and can indicate whether exercise triggers angina symptoms.
In some cases, imaging studies such as angiography may be necessary. This procedure involves the injection of a contrast dye into the coronary arteries, allowing for visualization of blood flow through the vessels via X-ray images. Angiography provides valuable information regarding blockages or narrowing that could lead to angina. Overall, accurate diagnosis is vital for determining the most effective treatment options and managing the condition effectively.
Treatment Options for Angina
Managing angina effectively often requires a multifaceted approach that includes lifestyle modifications, medications, and in some cases, invasive procedures. Each treatment plan should be tailored according to the specific needs of the patient, taking into consideration the severity of the condition and any underlying health issues.
One of the initial steps in treating angina typically involves lifestyle changes aimed at improving cardiovascular health. This may include adopting a heart-healthy diet, engaging in regular physical activity, maintaining a healthy weight, and quitting smoking. These modifications can significantly reduce the frequency and severity of angina episodes while promoting overall well-being.
In addition to lifestyle interventions, various medications play a critical role in the management of angina. Nitrates are commonly prescribed to relieve chest pain by dilating blood vessels and improving blood flow to the heart. Beta-blockers help reduce the heart’s workload and lower blood pressure, alleviating symptoms during exertion. Statins and other cholesterol-lowering drugs are also integral to angina treatment, as they decrease the risk of plaque buildup in the arteries, ultimately enhancing heart health and function.
When conservative measures are insufficient to control angina symptoms, more invasive procedures may be considered. Angioplasty, coupled with stenting, can help open up blocked arteries, restoring blood flow to the heart muscle. In cases of severe blockages or multiple arterial disease, coronary artery bypass grafting (CABG) may be recommended to reroute blood flow around the narrowed or obstructed arteries. Together, these interventions can provide significant relief for patients suffering from angina.
In summary, an effective angina treatment plan often combines lifestyle changes, medications, and potentially surgical interventions, emphasizing the importance of a personalized approach tailored to the patient’s unique circumstances and health status.
Lifestyle Changes to Manage Angina
Managing angina effectively often necessitates a holistic approach that integrates significant lifestyle changes. These changes can play a critical role in alleviating symptoms and minimizing the risk of further heart disease. A balanced diet is fundamental; incorporating fruits, vegetables, whole grains, lean proteins, and healthy fats can enhance overall cardiovascular health. Promoting heart-healthy eating habits may involve reducing salt, sugar, and saturated fat intake, which together can help control blood pressure and cholesterol levels, thus potentially mitigating angina symptoms.
Regular physical activity is another cornerstone of managing angina. Engaging in moderate exercise, such as walking, cycling, or swimming, can help improve heart function and build overall stamina. It is advisable for individuals with angina to consult healthcare professionals before initiating any exercise regimen, ensuring the activities chosen are appropriate and safe for their specific condition. Aim for structured exercise routines combined with daily physical movements to foster heart health.
Weight management also plays a crucial role in managing angina. Maintaining a healthy body weight helps reduce the strain on the heart, further alleviating angina symptoms. Combining a nutritious diet with regular exercise can facilitate effective weight control. Additionally, smoking cessation is vital. Smoking significantly increases the risk of heart disease and can exacerbate angina, thus, quitting can bring immediate and long-lasting benefits to cardiovascular health.
Stress management techniques, such as mindfulness meditation, yoga, or deep breathing exercises, can also be beneficial. Stress has been shown to impact heart health negatively, hence, adopting methods to alleviate stress is imperative for individuals with angina. Furthermore, regular medical check-ups to monitor heart health, adjust treatment plans, and foster lifestyle modifications can substantially contribute to managing angina and promoting overall health.
Preventing Angina: Strategies and Tips
Preventing angina requires a proactive approach towards maintaining heart health and addressing potential risk factors. One of the most effective strategies for preventing angina is to adopt a healthy lifestyle that includes regular physical activity, a balanced diet, and stress management techniques. Engaging in moderate aerobic exercise for at least 150 minutes per week can improve cardiovascular function and reduce the likelihood of heart-related conditions, including angina. Furthermore, a diet rich in fruits, vegetables, whole grains, and lean proteins helps manage weight and lower cholesterol levels, crucial factors in heart health.
Regular health screenings are vital for detecting risks and managing pre-existing conditions. Individuals should monitor blood pressure, cholesterol levels, and blood sugar regularly to maintain optimal cardiovascular health. It is also essential to address personal risk factors, such as smoking, diabetes, and obesity. Quitting smoking not only improves heart health but also enhances overall well-being. For those with diabetes, managing blood sugar levels effectively is necessary to minimize associated cardiovascular risks.
Education about the warning signs of angina can empower individuals to respond swiftly and effectively should symptoms arise. Typical symptoms include chest pain, shortness of breath, and fatigue. Recognizing these early signals and knowing when to seek medical attention can help mitigate more severe complications. It is advisable for individuals to consult health care professionals for personalized assessments and recommendations tailored to their specific needs.
Incorporating stress-reduction techniques such as mindfulness, yoga, or meditation can also significantly contribute to heart health. By understanding one’s risk factors and maintaining a balanced lifestyle, the likelihood of experiencing angina and other heart-related issues can be substantially diminished.

Living with Angina: Patient Experiences
Individuals living with angina often navigate a complex landscape of physical discomfort and emotional challenges. Many patients, upon being diagnosed, report feelings of uncertainty and anxiety regarding their condition. The experience of angina can vary greatly; some patients may encounter only mild discomfort, while others may face more severe episodes that disrupt daily life. Regardless of severity, managing angina requires a multidimensional approach that combines medical treatment, lifestyle modifications, and emotional support.
Patients have shared that adhering to a heart-healthy lifestyle plays a crucial role in managing symptoms. This includes engaging in regular, moderate exercise, maintaining a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, and quitting smoking if applicable. Many individuals find that tracking their symptoms, such as noting when angina episodes occur and their triggers, helps them anticipate and manage their condition more effectively.
Support systems also emerge as vital components in the lives of angina patients. Many join support groups, either in person or online, to connect with others who understand their journey. Sharing experiences helps to alleviate the sense of isolation that can come with chronic conditions. These collective environments not only foster emotional support but also provide practical coping strategies and resources. Additionally, mental health resources, including counseling or therapy, can help address feelings of anxiety and depression associated with the uncertainty of living with a chronic illness.
Furthermore, engaging in community activities with other patients or caregivers creates opportunities for both emotional and social support. Participating in exercise classes, educational workshops, or social gatherings can bolster a sense of belonging and equip individuals with the tools necessary to navigate life’s challenges while living with angina. These collective experiences showcase the resilience of those affected and their commitment to preserving quality of life in the face of adversity.
FAQ : Understanding Angina
What is angina?
Angina is chest pain or discomfort caused by reduced blood flow to the heart muscle, often a symptom of coronary artery disease.
What are the common symptoms of angina?
Symptoms include chest pain, pressure, tightness, or burning, often triggered by physical exertion or stress. Pain may also spread to the arms, neck, jaw, or back.
What are the different types of angina?
- Stable Angina: Occurs predictably with exertion and improves with rest.
- Unstable Angina: Unexpected and more severe, requiring urgent medical attention.
- Variant (Prinzmetal’s) Angina: Caused by coronary artery spasms, often occurring at rest.
What causes angina?
Angina is typically caused by coronary artery disease (CAD), where plaque buildup narrows the arteries. Other factors include high blood pressure, smoking, diabetes, and high cholesterol.
How is angina diagnosed?
Doctors may use tests like an ECG, stress test, echocardiogram, coronary angiography, or blood tests to diagnose angina.
How is angina treated?
Treatment options include lifestyle changes, medications (such as nitrates, beta-blockers, or statins), and procedures like angioplasty or bypass surgery for severe cases.
Can angina be prevented?
Yes, lifestyle changes like maintaining a healthy diet, regular exercise, quitting smoking, managing stress, and controlling blood pressure and cholesterol can help prevent angina.
Is angina life-threatening?
While stable angina is manageable, unstable angina can indicate an impending heart attack and requires immediate medical attention.
Can angina occur without chest pain?
Yes, some people—especially women, diabetics, and older adults—may experience angina as shortness of breath, fatigue, nausea, dizziness, or discomfort in areas like the jaw, neck, or arms without classic chest pain.
How long does an angina episode last?
Stable angina typically lasts a few minutes and goes away with rest or medication. If chest pain lasts longer than 10-15 minutes, worsens, or occurs at rest, it may be a sign of a heart attack and requires emergency medical attention.
What triggers angina pain?
Common triggers include physical exertion, emotional stress, cold weather, heavy meals, and smoking. Identifying and avoiding triggers can help manage symptoms.
How is angina different from a heart attack?
Angina is temporary chest pain caused by reduced blood flow but doesn’t cause heart muscle damage. A heart attack, however, involves blocked blood flow, leading to permanent heart damage. If angina symptoms become more severe or unpredictable, seek medical help immediately.
Can anxiety or stress cause angina?
Yes, stress and anxiety can trigger angina-like symptoms by increasing heart rate and blood pressure, reducing blood flow to the heart. Managing stress with relaxation techniques can help prevent episodes.
Can angina go away on its own?
Angina may subside with rest or medication, but the underlying heart condition remains. Ignoring angina symptoms is dangerous, as they may worsen over time. Always consult a doctor for proper diagnosis and treatment.
What medications are used to treat angina?
Common medications include:
- Nitrates (e.g., nitroglycerin) – to relax blood vessels and improve blood flow.
- Beta-blockers – to reduce heart rate and workload.
- Calcium channel blockers – to relax arteries and improve circulation.
- Antiplatelet drugs (e.g., aspirin) – to prevent blood clots.
- Statins – to lower cholesterol and prevent artery blockage.
Can angina be cured?
There’s no permanent cure for angina, but lifestyle changes, medications, and medical procedures can effectively manage it and prevent complications like heart attacks.
Is angina hereditary?
Yes, if you have a family history of heart disease, you may have a higher risk of developing angina. However, lifestyle choices play a major role in managing this risk.
Can I exercise if I have angina?
Yes, but under medical supervision. Moderate exercise strengthens the heart and improves circulation. However, avoid overexertion, and always follow your doctor’s recommendations.
Is angina more common in men or women?
Men are more likely to experience classic chest pain, while women often report unusual symptoms like nausea, breathlessness, or fatigue, making angina harder to diagnose in women.
Can diet affect angina?
Yes, a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can lower cholesterol and reduce angina risk. Avoid processed foods, excess salt, and saturated fats.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

