7 Shocking Facts About Tooth Decay You Must Know!
What is Tooth Decay?
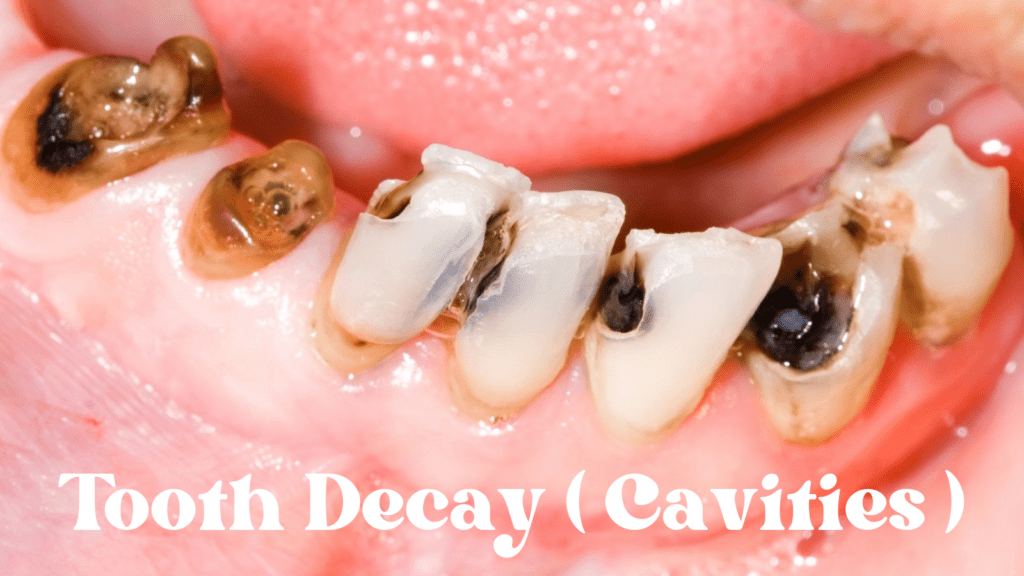
Tooth decay, also known scientifically as dental caries, is a multifactorial process characterized by the demineralization of tooth structure. This condition primarily results from the interplay of bacteria, dietary habits, and oral hygiene practices. The process begins when dental plaque, a sticky biofilm containing bacteria, accumulates on the teeth. If not adequately removed through regular brushing and flossing, these bacteria metabolize sugars present in the food and beverages we consume, producing acids as a byproduct.
The acids generated can erode the mineral content of the enamel, which is the outermost protective layer of the teeth. Initially, this demineralization may not cause any visible symptoms, but it is crucial to recognize that it sets the stage for more significant damage. As the process advances, the enamel begins to weaken, leading to early signs such as white spots on the tooth surface. If preventive measures are not undertaken at this stage, the decay progresses further, potentially resulting in cavitation, where significant structural loss occurs and cavities form.
Tooth decay can be classified into several stages, starting with initial demineralization, which is often reversible with proper dental care and fluoride treatment. However, as the decay progresses through stages such as enamel decay and dentin decay, the chances of recovery diminish, requiring dental interventions like fillings or crowns to restore the affected teeth. Understanding tooth decay is crucial for maintaining oral health, as it underscores the importance of good oral hygiene practices and regular dental check-ups geared toward prevention.
The Role of Bacteria in Tooth Decay
Tooth decay, or dental caries, is a multifactorial disease primarily driven by the presence of specific bacteria in the oral cavity. One of the most notorious culprits in this process is Streptococcus mutans, a bacterium that plays a pivotal role in the development of cavities. This microorganism thrives in the oral environment, particularly in the presence of fermentable sugars, which are abundantly found in many diets today.
Once sugars are consumed, S. mutans metabolizes these carbohydrates and produces acid as a byproduct. The acid generated from this bacterial activity can lead to the demineralization of tooth enamel, the protective outer layer of the teeth. This demineralization process, if left unchecked, can result in the formation of cavities, which are essentially permanent holes in the teeth.
In addition to S. mutans, other bacteria such as Lactobacillus species also contribute to the progression of tooth decay. These bacteria not only produce acids but can also enhance the cariogenic (cavity-causing) potential of plaque. Plaque is a sticky biofilm that forms on the surface of teeth, housing these bacteria and protecting them from the effects of saliva and oral hygiene practices. Over time, if this plaque is not adequately removed through regular brushing and flossing, it can harden into tartar, exacerbating the decay process.
The presence of these bacteria and their metabolic activities demonstrate the crucial role of microbiology in understanding tooth decay. Effective oral hygiene practices, including regular tooth brushing, flossing, and dental check-ups, are essential in controlling the bacterial load and mitigating the risk of developing cavities. By maintaining a balanced oral microbiome and minimizing sugar intake, individuals can significantly reduce their susceptibility to tooth decay.
Factors Contributing to Tooth Decay
Tooth decay, also known as dental caries, is a multifactorial disease influenced by various elements. Dietary choices play a crucial role in the development of cavities. The consumption of sugary foods and beverages is particularly detrimental, as sugars serve as a primary food source for the bacteria present in the mouth. These bacteria produce acids that can erode tooth enamel, leading to the formation of cavities. Reducing sugar intake can significantly decrease the risk of tooth decay and contribute to better oral health.
Oral hygiene practices are another essential factor in preventing cavities. Regular brushing and flossing remove food particles and plaque, which is a sticky film of bacteria that forms on teeth. Neglecting these practices can result in plaque buildup, allowing acids to attack the enamel over time. It is recommended to brush teeth at least twice daily with fluoride toothpaste and to floss at least once a day to maintain optimal oral hygiene and minimize the risk of decay.
Genetic predisposition can also affect an individual’s susceptibility to tooth decay. Some people may inherit enamel that is more porous or thinner, making their teeth more vulnerable to decay. Additionally, genetic factors could influence the composition of saliva, which plays a protective role against cavities by neutralizing acids and providing minerals that can remineralize enamel. Understanding one’s genetic background can be beneficial in assessing the risk of dental issues.
Lastly, systemic health conditions such as diabetes can significantly impact oral health. Individuals with diabetes often experience dry mouth due to reduced salivary flow, increasing the likelihood of cavity formation. Furthermore, high blood sugar levels can lead to oral infections and gum disease, which may create an environment conducive to tooth decay. Maintaining overall health through regular medical check-ups is essential not just for overall fitness, but for preserving oral health as well.

Stages of Tooth Decay: From Demineralization to Cavitation
Tooth decay is a gradual process that can lead to significant oral health issues if not addressed early. The initial stage of this process is known as demineralization, which begins when acids produced by bacteria in the mouth begin to erode the enamel. During this stage, white spot lesions appear on the enamel surface. These lesions are indicators that minerals, such as calcium and phosphate, are being lost, creating an opportunity for the decay to progress if left untreated.
If demineralization goes unaddressed, it can progress to the next stage, which involves the formation of cavities. At this point, the enamel’s structural integrity is compromised, leading to small holes or pits in the teeth. Cavities can vary in size and depth, and they often lead to increased sensitivity and discomfort. Once a cavity develops, it requires professional intervention, typically in the form of a dental filling, to restore the tooth and prevent further decay.
Early detection of tooth decay is vital in preventing its progression. Regular dental check-ups can identify white spot lesions before they advance to cavities, allowing for preventative measures to be taken. These measures may include fluoride treatments, dietary modifications, and improved oral hygiene practices. For example, fluoride can aid in the remineralization of early lesions while also strengthening the enamel against further acid attacks.
Moreover, understanding the stages of tooth decay emphasizes the importance of maintaining good oral hygiene habits. Brushing twice daily, flossing, and using mouthwash can significantly reduce the risk of plaque build-up and subsequent demineralization. By recognizing the signs of tooth decay early, individuals can make informed decisions regarding their dental health, ultimately preserving their teeth for a lifetime.
Preventing Tooth Decay: Effective Strategies
Tooth decay, commonly known as cavities, is a prevalent dental issue that can lead to significant oral health complications. However, the good news is that there are several effective strategies that individuals can adopt to prevent tooth decay and maintain optimal oral health. A key preventive measure is the practice of proper brushing and flossing techniques. It is recommended to brush twice a day with fluoride toothpaste and to replace toothbrushes every three months to ensure effective cleaning of the teeth and gums. Brushing should be performed in a circular motion to dislodge food particles and plaque effectively.
In addition to brushing, flossing is vital in preventing tooth decay. Flossing at least once a day helps remove plaque and food debris from between the teeth, where toothbrushes often cannot reach. This technique decreases the risk of cavities forming in these hard-to-reach areas. Furthermore, the importance of fluoride in oral health cannot be overstated. Fluoride helps strengthen tooth enamel, making it more resilient to decay. It can be obtained from fluoridated toothpaste, mouth rinses, or through professionally applied treatments at the dental office.
Diet modifications also play a crucial role in preventing tooth decay. Limiting sugary snacks and beverages, as well as acidic foods, can significantly reduce the risk of cavities. Instead, incorporating fruits, vegetables, whole grains, and dairy products into the diet provides essential nutrients while lowering the chances of decay. Regular dental check-ups are also essential; visiting the dentist at least twice a year allows for early detection and treatment of potential dental issues before they advance into serious problems.
By implementing these strategies, individuals can significantly diminish the risk of tooth decay and promote better oral health throughout their lives.
Treatment Options for Cavities
When addressing tooth decay, several treatment options are available, tailored to the severity of the condition. For early-stage cavities, fluoride treatments are often recommended. Fluoride, a naturally occurring mineral, aids in remineralizing enamel and can reverse the early stages of tooth decay. This method is particularly effective in children and adults who are at risk of developing cavities, as it strengthens the tooth’s surface and helps to prevent further decay.
As tooth decay progresses, more invasive procedures may become necessary. One common approach is dental fillings, utilized for cavities that have penetrated the enamel. During this procedure, the dentist removes the decayed portion of the tooth and fills the cavity with a material such as composite resin, amalgam, or glass ionomer. Fillings restore the tooth’s structure and function, while also preventing bacteria from further infecting the area.
For cavities that are more severe, crowns may be recommended. A dental crown encases the entire tooth, providing strength and protection after significant decay has occurred. This option is often used when a tooth is too damaged for a filling alone. The crown can be made from various materials, including porcelain or metal, depending on the location of the tooth and patient preferences.
In advanced cases of tooth decay, where infection has reached the pulp of the tooth, a root canal may be necessary. This procedure involves removing the infected pulp, cleaning the interior of the tooth, and sealing it to prevent reinfection. After a root canal, a crown is typically placed on the tooth to restore its function and appearance.
Ultimately, early detection and intervention through regular dental check-ups can significantly improve outcomes for those suffering from cavities. Understanding the range of treatment options available allows individuals to make informed decisions regarding their dental health.

The Impact of Tooth Decay on Overall Health
Tooth decay is often perceived as a localized dental issue; however, its implications extend far beyond the confines of oral health. Untreated cavities can serve as gateways for bacteria, leading to infections that not only affect the mouth but can also spread to other parts of the body. For instance, dental abscesses, which are infective pockets that may develop as a result of profound tooth decay, can require urgent medical attention to prevent more serious health consequences. If left unresolved, these infections can permeate the bloodstream, leading to conditions such as sepsis, which poses a life-threatening risk.
Moreover, numerous studies have established a compelling link between oral health and systemic diseases. For example, the presence of chronic gum disease and cavities are strongly associated with cardiovascular disease. The rationale behind this connection is that oral bacteria can enter the bloodstream and ultimately contribute to inflammation—a significant factor in heart disease. Similarly, recent research has indicated that individuals with tooth decay and periodontal disease may have a higher risk of developing diabetes, as poor oral health can affect glucose levels and insulin function.
The ramifications of tooth decay are not limited to immediate health concerns; they can have profound implications for an individual’s quality of life. Pain from cavities can hinder one’s ability to eat, speak, and even concentrate, which may lead to nutritional deficiencies and psychological stress. Furthermore, social interactions can be adversely affected, especially when issues such as bad breath or visible decay become apparent. This interaction underlines the importance of a holistic approach to health, wherein maintaining good oral hygiene is vital not only for preserving teeth but also for safeguarding overall health.
Common Myths about Tooth Decay
Tooth decay, a prevalent dental issue, is often surrounded by various misconceptions that can hinder effective preventive practices. One widely held belief is that only sugary foods can lead to cavities. While it is true that sugar plays a significant role in the formation of cavities, other carbohydrates, like bread and pasta, can also contribute to tooth decay. These foods, when broken down, can create an acidic environment in the mouth, promoting bacteria growth. This highlights the importance of a well-rounded approach to dietary choices and not solely focusing on sugars.
Another common myth is the idea that brushing teeth is unnecessary if one does not experience pain. Many individuals tend to neglect their oral hygiene under the assumption that the absence of discomfort indicates healthy teeth. However, cavities can develop silently, often without noticeable symptoms until they reach an advanced stage requiring significant intervention. Regular brushing, even in the absence of pain, is essential for removing food particles and bacteria, thus preventing the progression of tooth decay.
Additionally, some people believe that dental treatments can serve as a complete substitute for proper oral care. While procedures like fillings or crowns are effective in repairing damage caused by decay, they do not eliminate the underlying causes. Consistent oral hygiene practices, including daily brushing and flossing, along with regular dental check-ups, remain crucial for maintaining oral health and preventing cavities. Understanding these myths and recognizing the facts about tooth decay can empower individuals to make informed decisions regarding their oral care, ultimately leading to healthier teeth and gums.
Frequently Asked Questions (FAQs) about Cavities
Tooth decay, commonly resulting in cavities, raises numerous questions among individuals seeking to understand its implications. Here, we address some of the most frequently asked questions related to cavities and provide insights into prevention and treatment options.
How often should I visit the dentist?
Regular dental visits are crucial for maintaining oral health. It is generally recommended to visit the dentist at least twice a year for check-ups and cleanings. However, individuals with a higher risk of developing cavities due to factors like previous dental issues, poor oral hygiene, or dietary habits may need to schedule more frequent visits. Your dentist can establish a personalized schedule based on your specific needs.
What symptoms should I watch for?
Cavities develop over time and may not always present obvious symptoms initially. However, some signs of tooth decay include tooth sensitivity, pain when biting or chewing, visible holes or pits in teeth, and discoloration. If you experience these symptoms, it is advisable to consult a dentist promptly to prevent further damage.
What treatments are available for cavities?
The treatment for cavities varies depending on their severity. Early-stage cavities, which are often detectable by a dentist, may be treated with fluoride treatments or dental sealants to restore enamel. For more advanced decay, restorative treatments such as fillings, crowns, or root canals may be necessary. It is essential to address tooth decay promptly to avoid complications and maintain overall dental health.
Are there preventive measures I can take?
Good oral hygiene practices can significantly reduce the risk of developing cavities. Brushing twice a day with fluoride toothpaste, flossing daily, and limiting sugary snacks can all help protect against tooth decay. Additionally, incorporating regular dental cleanings and being aware of changes in your oral health can further enhance prevention efforts.
By understanding these common questions about cavities, individuals can take proactive steps to maintain oral health and seek appropriate treatment when necessary.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

