Bone Marrow Health: 5 Unique Insights for Strength
Understanding Bone Marrow Health
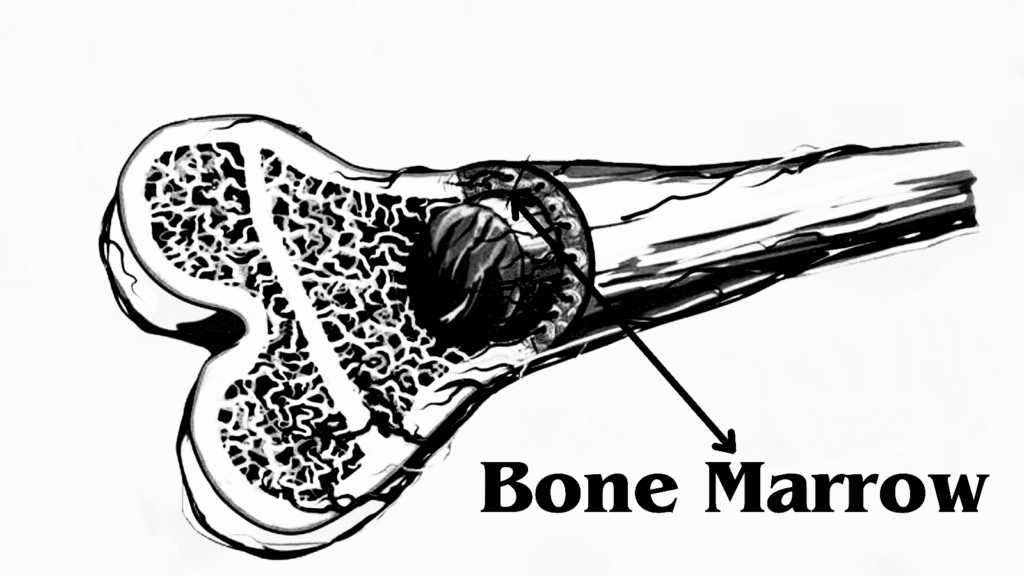
Bone marrow is a vital, spongy tissue located within the cavities of bones, predominantly found in the larger bones of the human body such as the pelvis, ribs, sternum, and long bones of the limbs. Its primary function is to produce blood cells, making it essential for the maintenance of a healthy circulatory system. Bone marrow can be categorized into two distinct types: red marrow and yellow marrow, each serving unique functions.
Red marrow, also known as myeloid tissue, is richly populated with hematopoietic stem cells, which are responsible for generating various types of blood cells, including red blood cells, white blood cells, and platelets. This type of marrow gives blood its characteristic color and plays a crucial role in the overall metabolic processes within the body. In contrast, yellow marrow primarily consists of adipose (fat) tissue and serves as a reserve for energy. Under certain circumstances, such as severe blood loss or increased demand for blood cell production, yellow marrow can convert back to red marrow, underscoring its adaptability.
Structurally, bone marrow features a complex network of stromal cells, extracellular matrix, and blood vessels, all of which provide the necessary microenvironment for hematopoiesis—the formation of blood cells. The composition of bone marrow changes with age; in infants, nearly all marrow is red, while in adults, the proportion of yellow marrow increases. Additionally, bone marrow plays a pivotal role in the immune system, as it generates various immune cells that protect the body from infections and diseases. Therefore, the health and functionality of bone marrow are crucial for the overall well-being and resilience of the human body.
Types of Bone Marrow and Their Functions
Bone marrow is primarily classified into two main types: red marrow and yellow marrow, each serving distinct yet essential functions within the body.
Red marrow, also known as myeloid tissue, plays a critical role in the process of hematopoiesis, which is the formation of blood cells. This type of marrow is predominantly found in flat bones such as the pelvis, sternum, and the ribs, as well as in the epiphyses of long bones. In red marrow, stem cells generate erythrocytes (red blood cells), leukocytes (white blood cells), and thrombocytes (platelets). The production of these cells is vital for various physiological functions, including oxygen transport, immune response, and blood clotting. The active nature of red marrow makes it a key player in maintaining the body’s homeostasis by responding dynamically to the organism’s needs, especially during times of stress or blood loss.
Conversely, yellow marrow serves a different purpose, primarily functioning as a storage site for fats, or adipocytes. It is mainly found in the medullary cavities of long bones, such as the femur and humerus. Although yellow marrow does not produce blood cells, it can be converted back into red marrow if necessary, particularly in cases of severe anemia or other conditions requiring increased blood cell production. This adaptability underscores the importance of yellow marrow within the hematopoietic system. The presence of reserves in the form of fat is crucial for energy storage, impacting overall metabolic health.
Both types of bone marrow are vital for sustaining life and ensuring the proper functioning of the immune and circulatory systems. Understanding these functions provides insight into the intricate workings of the human body and highlights the importance of maintaining healthy bone marrow.
The Role of Bone Marrow in the Immune System
Bone marrow serves a critical function within the immune system, acting as the primary site for the production of lymphocytes and other essential immune cells. It is in the bone marrow where hematopoiesis, the process of blood cell formation, occurs. This intricate process produces not only red blood cells and platelets but also white blood cells, which play pivotal roles in the body’s defense mechanisms against pathogens.
Among the various types of white blood cells, lymphocytes, including T cells and B cells, are particularly significant. T cells are responsible for directly attacking infected cells, while B cells produce antibodies that neutralize pathogens. The maturation and differentiation of these lymphocytes occur primarily in the bone marrow, showcasing its essential role in establishing a competent immune response. A deficiency in bone marrow function can lead to a compromised immune system, making the body more susceptible to infections and diseases.
Furthermore, the bone marrow also produces other crucial cells such as granulocytes and monocytes, which are involved in the inflammatory response and the clearance of pathogens. The health of the bone marrow directly correlates with the overall performance of the immune system. Factors such as age, disease, or environmental stressors can adversely affect bone marrow health, thereby impairing its ability to produce lymphocytes and other immune components.
A healthy and functional bone marrow is paramount for a robust immune system, as it ensures an adequate supply of immune cells necessary for the detection and elimination of infections. As such, maintaining bone marrow health is essential not only for the immune system but also for overall health and well-being. Understanding the integral role of bone marrow is vital for acknowledging how it supports the body’s defenses against disease.

Bone Marrow Disorders: Overview and Types
Bone marrow disorders encompass a variety of medical conditions that can significantly affect the functionality of the bone marrow. They can disrupt the production of blood cells, leading to serious health complications. Among the most prevalent disorders are leukemia, aplastic anemia, and myelodysplastic syndromes. Each of these conditions has unique characteristics and symptoms which warrant an in-depth understanding.
Leukemia is a type of cancer that primarily impacts the bone marrow and blood, causing the production of abnormal white blood cells. These dysfunctional cells can crowd out healthy blood cells, leading to symptoms such as fatigue, frequent infections, and easy bruising or bleeding. Leukemia can broadly be classified into acute and chronic forms, impacting both adults and children, with varying prevalence among different age groups.
Aplastic anemia is another serious disorder characterized by the insufficient production of blood cells due to damage to the bone marrow. This condition can arise from environmental factors, autoimmune diseases, or viral infections. Symptoms of aplastic anemia include prolonged fatigue, higher susceptibility to infections, and an increased tendency to bleed or bruise easily. This disorder necessitates timely intervention, as its severity can escalate rapidly without treatment.
Myelodysplastic syndromes (MDS) represent a group of disorders caused by poorly formed or dysfunctional blood cells, resulting from problems in the bone marrow. Patients suffering from MDS may experience symptoms such as anemia, high risk of infections, and bleeding tendencies. MDS can progress to acute myeloid leukemia, making early diagnosis and management crucial.
Other notable disorders affecting bone marrow functionality include multiple myeloma and sickle cell disease. Each of these disorders highlights the critical nature of bone marrow health and its direct correlation with overall well-being. Addressing these conditions through appropriate medical interventions can significantly improve patients’ quality of life.
Diagnosis of Bone Marrow Conditions
Diagnosing bone marrow conditions is a critical process that enables healthcare professionals to identify various disorders affecting the marrow’s health and functionality. Bone marrow, being a vital component of the hematopoietic system, requires precise diagnostic techniques to uncover potential abnormalities. The most commonly utilized methods include bone marrow biopsy, aspiration, and advanced imaging studies.
A bone marrow biopsy is an essential procedure where a small sample of bone marrow is extracted for examination under a microscope. This technique allows the pathologist to investigate the cellularity, individual cell types, and the overall architecture of the bone marrow. It is particularly useful in diagnosing conditions such as leukemia, lymphoma, and myelodysplastic syndromes. Additionally, it helps determine the stage of certain cancers and assess the extent of metastasis.
Bone marrow aspiration often accompanies a biopsy. During this procedure, a thin needle is inserted into the bone, typically the hip bone, to collect a liquid sample of the marrow. This fluid contains hematopoietic cells that can be analyzed for abnormalities, infection, or malignancy. Aspiration is especially valuable in evaluating conditions such as anemias, thrombocytopenias, and leukemias, where understanding the composition of blood cells is crucial for diagnosis.
Imaging studies also play a vital role in the diagnostic process. Techniques like magnetic resonance imaging (MRI) and computed tomography (CT) scans can provide important insights into the morphology of the bone marrow and surrounding structures. These imaging modalities help assess changes related to infiltration from cancers or other diseases and can guide decisions regarding further invasive procedures.
In conclusion, accurate diagnosis of bone marrow conditions relies on a combination of procedures, including biopsies, aspirations, and imaging studies. Each technique contributes uniquely to understanding the underlying issues in various bone marrow disorders, ultimately guiding physicians in selecting the most appropriate treatment options.
Treatments for Bone Marrow Disorders
Bone marrow disorders encompass a range of conditions affecting blood cell production and overall bone marrow function. Due to the critical role of bone marrow in hematopoiesis, targeted treatments are essential for managing these disorders. The primary treatment approaches include chemotherapy, radiation therapy, stem cell transplants, and supportive care, each possessing unique mechanisms and considerations for patient selection.
Chemotherapy is frequently employed to treat various bone marrow disorders, particularly those classified as hematological malignancies such as leukemia and lymphoma. This treatment utilizes cytotoxic drugs to eradicate rapidly dividing cancer cells. The selection of specific chemotherapeutic agents depends on the type of disease, its stage, and the patient’s overall health. While chemotherapy can be effective, it often comes with adverse effects that require careful management.
Radiation therapy is another option, which involves the use of high-energy particles or waves to destroy cancer cells or halt their growth. It can be particularly beneficial in reducing the size of tumors in patients with localized bone marrow disorders. Like chemotherapy, radiation therapy may present side effects, necessitating a thorough evaluation of the benefits versus risks for each individual patient.
Stem cell transplants, or hematopoietic stem cell transplants, represent a more advanced treatment modality, especially for patients with severe bone marrow disorders or those who have failed other therapies. This procedure involves replacing diseased or damaged bone marrow with healthy stem cells, either from the patient or a donor. Success rates are influenced by various factors, including the source of the stem cells and the patient’s age and general health.
Lastly, supportive care plays a critical role in managing symptoms and maintaining quality of life. This may include blood transfusions, growth factor therapies, and pain management strategies. Understanding the available therapeutic options allows healthcare providers to tailor treatments to the specific needs of patients suffering from bone marrow disorders, maximizing both effectiveness and safety.

Bone Marrow Transplantation: Procedures and Advances
Bone marrow transplantation is a critical medical procedure designed to treat various hematologic diseases, including leukemia, lymphoma, and aplastic anemia. The transplantation process involves replacing damaged or diseased bone marrow with healthy marrow. This can be achieved through two primary types of transplants: autologous and allogeneic. An autologous transplant utilizes the patient’s own bone marrow or stem cells, while an allogeneic transplant involves marrow taken from a genetically compatible donor.
The procedure begins with extensive pre-transplant evaluations, including blood tests and imaging studies to determine the patient’s overall health and suitability for the transplant. If an allogeneic transplant is necessary, identifying a compatible donor is crucial. This matching process includes analyzing human leukocyte antigen (HLA) markers to ensure the best fit between the donor and patient. Once a donor is found, both the patient and donor undergo several preparatory treatments. These typically involve chemotherapy or radiation therapy aimed at eradicating any remaining diseased cells in the patient’s bone marrow, allowing for a better chance of successful engraftment of the new cells.
Following the transplant, patients enter a recovery phase where they are monitored closely for potential complications such as infections or graft-versus-host disease (GVHD), a condition where transplanted cells attack the recipient’s tissues. Advances in transplantation techniques, such as enhanced donor matching protocols and improved conditioning regimens, have significantly increased the rates of successful outcomes. Furthermore, innovative technologies like cord blood and peripheral blood stem cell transplants have expanded the options available to patients requiring bone marrow transplants. These developments in transplantation methods continue to revolutionize treatment approaches, underscoring the importance of ongoing research in the field.
Nutritional Influences on Bone Marrow Health
The health of bone marrow is significantly influenced by nutrition, as the marrow serves as a vital site for hematopoiesis, the production of blood cells. Adequate intake of specific nutrients is crucial for maintaining optimal bone marrow function and overall hematological health. Key nutrients that support the robust operation of the bone marrow include vitamins B12, B6, folate, and essential minerals such as iron, zinc, and copper.
Vitamin B12, found abundantly in animal products such as fish, meat, and dairy, plays a crucial role in the formation of red blood cells. Its deficiency can lead to anemia, consequently affecting bone marrow health adversely. Similarly, folate, which is readily available in leafy greens, legumes, and fortified cereals, is paramount for the synthesis of nucleic acids and contributes significantly to the production of healthy blood cells. Vitamin B6 also plays an essential role in hemoglobin formation and is present in various foods, including poultry, fish, potatoes, and non-citrus fruits.
Iron is another essential nutrient that supports bone marrow health, as it is a key component of hemoglobin, which carries oxygen in the blood. Iron-rich foods like red meat, beans, and lentils should be incorporated into a balanced diet to prevent deficiencies that can impede bone marrow activity. Additionally, minerals such as zinc and copper contribute to the functioning of various enzymes involved in hematopoiesis, making them important for maintaining a healthy bone marrow environment.
A balanced diet that includes a variety of fruits, vegetables, whole grains, and lean proteins will provide the necessary nutrients to ensure optimal bone marrow health. Adequate hydration and the avoidance of excessive alcohol and processed foods also contribute to a conducive environment for bone marrow function and overall health.
Frequently Asked Questions About Bone Marrow
Bone marrow is a crucial component of the human body, serving essential functions in blood cell production and the immune system. Understanding its role can raise several questions, and below, we address some of the most common inquiries related to bone marrow.
What is the primary function of bone marrow?
The primary function of bone marrow is to produce hematopoietic cells, which lead to the generation of red blood cells, white blood cells, and platelets. This process, known as hematopoiesis, is vital for maintaining healthy blood circulation and a functional immune response. The red blood cells carry oxygen, while white blood cells are integral to fighting infections.
How does lifestyle affect bone marrow health?
Lifestyle factors significantly influence the health and functionality of bone marrow. A balanced diet rich in vitamins and minerals, particularly folate, vitamin B12, and iron, is essential for optimal hematopoiesis. Regular exercise can also enhance circulation, which indirectly benefits bone marrow function. Conversely, habits such as smoking, excessive alcohol consumption, and a sedentary lifestyle can negatively impact bone marrow, leading to various health issues.
What conditions can affect bone marrow?
Several medical conditions can impact bone marrow health, including leukemia, aplastic anemia, and myelodysplastic syndromes. These disorders may result in insufficient production or dysfunctional blood cells, leading to severe consequences for the individual’s overall health. Symptoms may include fatigue, frequent infections, and easy bruising. It is crucial to seek medical advice if any concerning signs arise, as early diagnosis can significantly improve treatment outcomes.
What are the signs of bone marrow problems?
Bone marrow problems can present through various symptoms, depending on the underlying condition. Common signs include unexplained fatigue, frequent infections, bruising or bleeding easily, and shortness of breath. These symptoms often occur due to a decrease in blood cell production. If you experience any of these symptoms, it’s important to seek medical attention promptly for an accurate diagnosis and appropriate treatment.
Can bone marrow recover from damage?
Bone marrow has a remarkable ability to recover from certain types of damage, especially if caught early. For example, bone marrow suppression caused by chemotherapy may improve over time with the right medical intervention. However, in some conditions like severe aplastic anemia or certain cancers, bone marrow damage may be permanent, and treatment such as a bone marrow transplant may be necessary. The extent of recovery depends on the severity and cause of the damage.
In summary, understanding the role and function of bone marrow is essential for optimal health. By addressing common queries, we can clarify misconceptions and highlight the importance of maintaining this critical component of the human body.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

