How Mastectomy Saves Lives: 6 Powerful Insights
What is Mastectomy?
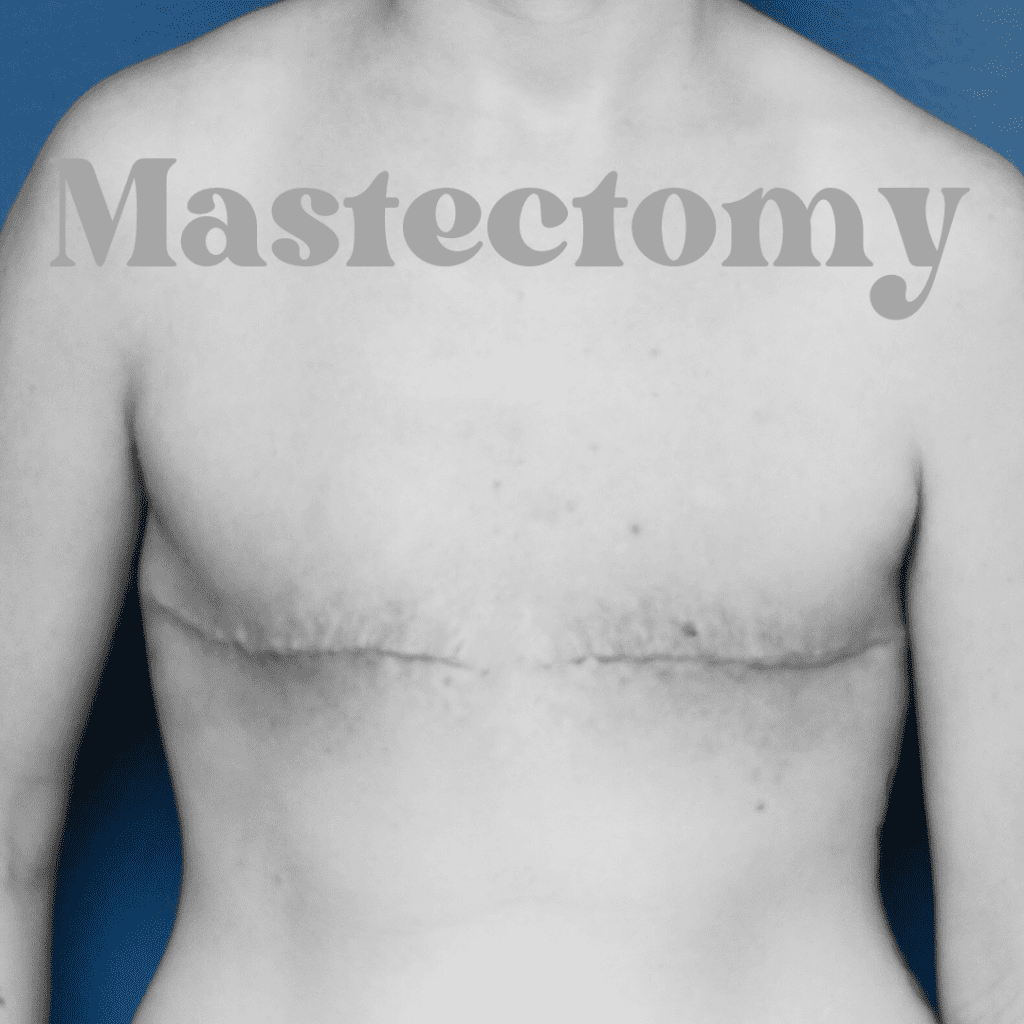
Mastectomy is a surgical procedure that involves the removal of one or both breasts, commonly performed as a treatment for breast cancer. This procedure can be a critical component in managing and preventing the spread of cancerous cells and can significantly impact a patient’s prognosis. Mastectomy is not limited to cancer treatment; it is also utilized in cases where a patient exhibits a high genetic risk for breast cancer, such as those with BRCA1 or BRCA2 gene mutations. By removing breast tissue, the procedure aims to minimize the likelihood of developing malignancies in the future.
There are several types of mastectomy, each tailored to the individual needs of the patient and the extent of the disease. The total mastectomy, also known as a simple mastectomy, involves the complete removal of the breast along with its skin, nipple, and areola. This is often employed when the cancer is extensive or if there are concerns regarding the margins that may remain after a less invasive operation. In contrast, a partial mastectomy, or lumpectomy, entails the surgical removal of the tumor and a small margin of surrounding healthy tissue. This option is typically considered for early-stage cancers, where breast conservation is desired.
Other variations include the modified radical mastectomy, which combines the total removal of the breast with the removal of lymph nodes in the underarm area, and the skin-sparing mastectomy, which removes the breast tissue but preserves most of the skin to facilitate future reconstructive options. These varying surgical choices underscore the importance of personalized treatment plans. Ultimately, the decision to undergo a mastectomy, and the specific type of surgery, is informed by a combination of medical advice, patient preferences, and the contextual specifics of the diagnosis.
Types of Mastectomy
Mastectomy is a surgical procedure aimed at the removal of one or both breasts, typically conducted as a treatment for breast cancer or as a preventive measure in high-risk patients. There are several types of mastectomy, each with unique indications, surgical approaches, and implications for patient recovery.
The most commonly performed mastectomy is the total mastectomy, which involves the complete removal of the breast tissue, including the nipple and areola. This type is usually recommended for women diagnosed with invasive breast cancer, particularly when the tumor is large or when there are multiple areas of cancer in the breast. The total mastectomy ensures that all potentially affected tissue is excised, reducing the risk of cancer recurrence.
Another type is the partial mastectomy, often referred to as lumpectomy or segmental mastectomy. This procedure removes only the tumor and a margin of surrounding healthy tissue. It is considered for patients with small tumors and is typically accompanied by radiation therapy. This approach aims to conserve as much breast tissue as possible while ensuring effective treatment.
Radical mastectomy involves the removal of the entire breast, underlying chest muscle, and surrounding lymph nodes. While this procedure was once the standard for advanced breast cancer, it is now rare due to the more conservative approaches available. Patients undergoing radical mastectomy may experience greater physical changes and require a longer recovery period compared to other types.
Finally, the prophylactic mastectomy is a preventive measure taken by women with a very high risk of developing breast cancer, often due to genetic factors such as BRCA1 or BRCA2 mutations. This procedure can significantly reduce the risk of cancer but carries emotional and physical implications that must be carefully considered.
Each type of mastectomy has its own set of indications, surgical techniques, and recovery pathways, ultimately tailored to the individual needs of the patient. Understanding these differences is crucial for informed decision-making regarding breast health and cancer treatment.
Reasons for Mastectomy
Mastectomy, which involves the surgical removal of one or both breasts, is primarily performed as a treatment for breast cancer. The decision to undergo this procedure often stems from various medical reasons, primarily centered around the presence of cancerous tissue. When diagnosed with breast cancer, one significant factor to consider is the tumor’s size and location. Larger tumors or those that have spread can lead to the recommendation for mastectomy over lumpectomy in order to ensure the complete removal of cancerous cells.
Additionally, the stage of cancer plays a crucial role in determining the most suitable course of action. For women diagnosed with stage II or III breast cancer, mastectomy may be deemed necessary to minimize the risk of recurrence. Furthermore, individuals exhibiting particular risk factors—such as family history—might consider mastectomy as a preventive measure. Genetic predispositions, notably mutations in the BRCA1 or BRCA2 genes, significantly increase a person’s likelihood of developing breast cancer. For these individuals, prophylactic mastectomy may represent a proactive approach toward reducing the risk of future malignancies.
Beyond genetic considerations, personal health decisions significantly shape the choice to undergo mastectomy. Women may opt for this procedure to alleviate anxiety about potential cancer resurgence, seeking peace of mind and improved quality of life. Moreover, the effectiveness of mastectomy in achieving clear surgical margins enhances its consideration among healthcare professionals and patients alike. This technique may also serve as a therapeutic step prior to or following other treatments, such as chemotherapy or radiation, emphasizing its integral role within the broader context of breast cancer management. Ultimately, the decision for mastectomy should involve careful deliberation and thorough discussions between patients and their healthcare teams.

The Mastectomy Procedure
The mastectomy procedure is a critical surgical intervention used primarily for the treatment of breast cancer. Before the operation, patients undergo various pre-operative preparations, which may include imaging tests, physical examinations, and consultations to explain the surgical process. These preparations are essential to ensure that patients have a clear understanding of the procedure and to address any concerns they might have.
On the day of the surgery, patients are typically administered general anesthesia, ensuring that they remain unconscious and pain-free throughout the operation. This approach allows the surgeon to perform an extensive mastectomy, which may involve the removal of one or both breasts, depending on the case’s specific requirements. The surgical team consists of experienced professionals, including the surgeon, anesthesiologist, and nursing staff, all of whom play an integral role in the patient’s care during the procedure.
During the operation, a variety of techniques can be employed, including total, modified radical, or partial mastectomy. The choice of technique depends on the type and stage of breast cancer being treated. Generally, the surgeon begins by making strategic incisions to access the breast tissue, lymph nodes, and surrounding structures. The tissue is carefully removed, ensuring that clear margins are obtained, which is crucial for reducing the risk of cancer recurrence. The entire procedure typically lasts between one to three hours, although this may vary based on individual factors.
After the mastectomy, patients are closely monitored in a recovery room. They can expect to experience some discomfort and swelling but will receive pain management interventions as needed. Instructions for post-operative care, including how to care for the surgical site and signs of complications, will be provided to ensure a smooth recovery. This comprehensive approach not only emphasizes the meticulous nature of the mastectomy procedure but also reinforces the importance of the surgical team in providing optimal patient care.
Recovery After Mastectomy
Recovery following a mastectomy is a critical phase that influences a patient’s physical and emotional well-being. The healing process begins immediately after surgery, where effective pain management is paramount. Surgeons typically prescribe analgesics to manage discomfort, which can vary in intensity depending on the individual. Patients are encouraged to communicate openly about their pain levels, enabling healthcare providers to tailor pain relief strategies that ensure comfort during recovery.
Wound care also plays a vital role in the recovery process. Patients should receive detailed instructions on how to care for their incisions, which may include keeping the area clean and dry, changing dressings as directed, and monitoring for any signs of infection, such as increased redness, swelling, or discharge. Moreover, understanding potential complications like seromas and hematomas is essential for early detection and management, contributing to a smoother recovery.
As healing progresses, many patients begin to consider the return to their daily activities. While some may regain their normal routines within weeks, others might require additional time to adjust. It is important to gradually reintroduce physical activities, starting with light exercises to maintain mobility and strength. Adhering to a healthcare provider’s guidance is crucial for ensuring a safe resumption of activities.
Follow-up care constitutes an integral component of post-mastectomy recovery. Regular check-ups allow healthcare professionals to monitor the healing process and address any emerging concerns. This ongoing relationship with medical providers helps identify any psychological or physical challenges related to the surgery. Overall, patient awareness and dedication to recovery significantly enhance health outcomes, reinforcing the necessity of meticulous health monitoring during this critical period.
Reconstruction Options Post-Mastectomy
Breast reconstruction after a mastectomy offers individuals a pathway to regain their sense of self and improve their quality of life. Various options are available, which can be categorized into surgical and non-surgical methods. Surgical options primarily include immediate or delayed reconstruction utilizing implants or autologous tissue, while non-surgical options often encompass the use of external prosthetics.
Immediate reconstruction occurs simultaneously with the mastectomy, offering the benefit of fewer surgeries and a more integrated recovery experience. This method typically employs breast implants or tissue expanders to create a breast mound. Conversely, delayed reconstruction allows individuals to focus on their recovery from surgery and any subsequent treatments, such as chemotherapy or radiation therapy, before considering reconstruction. This option might involve using the patient’s own tissue from areas such as the abdomen or back, which can provide a natural feel and appearance.
When considering reconstruction, timing plays a significant role. Surgeons often assess the individual’s overall health, treatment plan, and personal preferences. Factors that influence decision-making include the type of mastectomy performed, the presence of cancer in the lymph nodes, and the psychological impact of reconstructive surgery on the individual. Consulting with a multidisciplinary team, including oncologists and plastic surgeons, can provide valuable insights and assist in making an informed choice.
Aside from surgical options, many individuals prefer non-surgical solutions, especially if they encounter difficulties with recovery or prefer not to undergo additional surgeries. External prosthetics are designed to mimic the appearance of natural breasts and can be easily worn with various types of clothing. This option offers an immediate solution without surgical risks or complications.
Ultimately, the choice of reconstruction is a personal one, shaped by individual circumstances, preferences, and medical advice. Engaging in thorough discussions with healthcare providers can lead to an empowered decision-making process, reflecting the individual’s desires and health needs.

Emotional and Psychological Impact
A mastectomy is not only a physical procedure; it brings with it significant emotional and psychological implications for patients. The feelings of loss can be overwhelming, as individuals grapple with the removal of a breast, which may be synonymous with femininity and self-identity. Many women express a profound sense of grief, likening the experience to mourning the loss of a part of themselves. This emotional response is a natural reaction to the trauma of significant changes in one’s body.
Body image issues frequently arise in the wake of a mastectomy. Patients may struggle with their self-esteem and confidence, feeling that they no longer align with societal standards of beauty. This shift can lead to anxiety, depression, or a sense of isolation. Furthermore, the physical scars left after surgery can serve as constant reminders of their health battle, impacting one’s self-perception and overall well-being.
Coping strategies become vital during this challenging time. Engaging in support groups allows women to share their experiences with others who understand their struggles, fostering a sense of community and belonging. Professional counseling or therapy may also prove beneficial; mental health professionals can provide tailored strategies to help navigate these complex feelings. Techniques such as mindfulness, meditation, or yoga can further assist in managing stress and promoting emotional healing.
It is essential for patients to seek and accept mental health support during their recovery journey. Resources, such as hotlines, online forums, and local support networks, offer vital assistance and varying perspectives on navigating post-mastectomy life. Adequate attention to emotional well-being is critical, as it can enhance overall recovery and quality of life. By prioritizing mental health, patients can embark on a path towards resilience, acceptance, and healing after surgery.
Frequently Asked Questions (FAQs)
Mastectomy is a significant surgical procedure, and it is natural for patients to have numerous questions and concerns. Here are some common queries that many individuals ask about the mastectomy process.
What can I expect in terms of pain after a mastectomy?
Pain levels can vary greatly from person to person. Typically, patients may experience discomfort or pain for several days post-surgery, managed effectively with prescribed pain medication. The intensity of pain often decreases over time, and physical therapy is often recommended to aid recovery and reduce discomfort.
How long does recovery take after a mastectomy?
The recovery timeframe can vary based on the type of mastectomy performed and the individual’s overall health. Generally, patients may stay in the hospital for one to two nights. The initial healing period usually lasts about two weeks, during which patients should limit physical activity. Full recovery may take several weeks, with most individuals returning to normal activities within six to eight weeks.
Will mastectomy affect my fertility?
For most women, a mastectomy does not directly affect fertility; however, if additional treatments, such as chemotherapy or radiation, are required, they may influence fertility levels. It is vital for patients to discuss concerns about fertility with their healthcare provider before undergoing surgery, as there are options available for fertility preservation.
What is the impact of mastectomy on sexual health?
The impact of mastectomy on sexual health varies among individuals. Physically, some may experience changes in sensation or a shift in body image, which can affect intimacy and sexual relations. It is essential to have open discussions with partners and healthcare providers about these concerns. Many find support groups or counseling beneficial to address emotional aspects of intimacy post-mastectomy.
How will a mastectomy affect my daily life?
After a mastectomy, many individuals can return to their usual daily routines, though there may be a period of adjustment. Initially, you may need to modify activities such as lifting heavy objects or strenuous exercise to allow the body to heal. Most individuals gradually regain their independence, but it’s important to follow your surgeon’s guidance and take time for self-care during recovery.
Are there options for breast reconstruction after a mastectomy?
Yes, breast reconstruction is an option for many individuals after a mastectomy. This can be done using implants or by using tissue from other parts of the body (autologous reconstruction). The decision depends on various factors, including health, personal preference, and the advice of your healthcare team. It is recommended to discuss your options with a reconstructive surgeon before or after the mastectomy to determine what’s best for you.
Understanding these factors can help prepare individuals for the changes that may arise following a mastectomy and enable them to seek appropriate support during their recovery journey.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

