Understanding Lung Cancer: 7 Key Insights for Hope
Understanding Lung Cancer
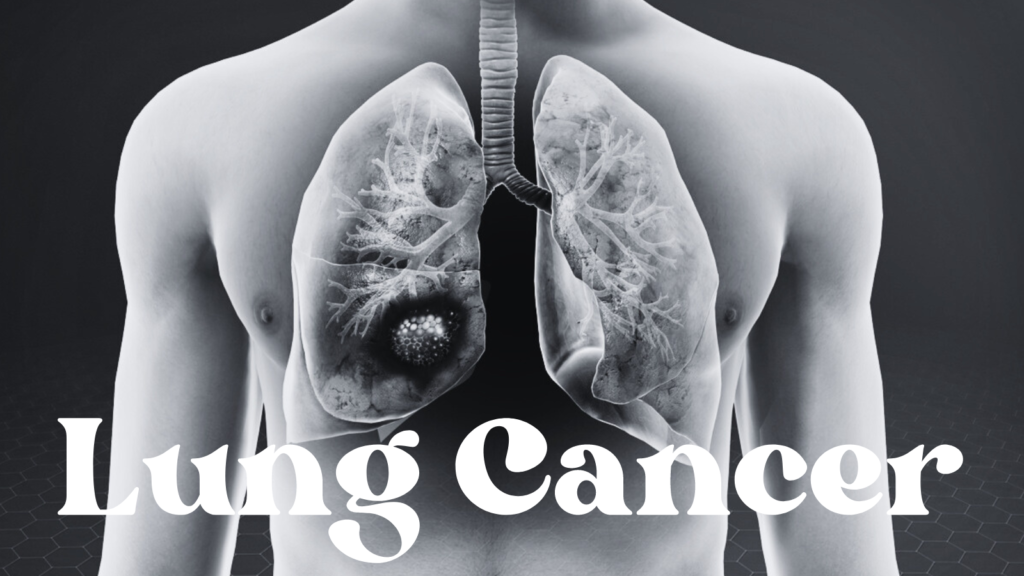
Lung cancer is characterized by the uncontrolled growth of abnormal cells in the lung tissue. These malignant cells can form tumors, which may invade and damage surrounding lung tissues and organs. Lung cancer is a leading cause of cancer-related mortality globally, emphasizing its significant impact on public health. This type of cancer is primarily classified into two main categories: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Each type demonstrates different characteristics, treatment responses, and prognoses.
Non-small cell lung cancer accounts for approximately 85% of all lung cancer cases. This category comprises several subtypes, including adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Given its prevalence, NSCLC is often diagnosed at a more advanced stage, thus complicating treatment options. On the contrary, small cell lung cancer represents about 15% of cases and is known for its rapid growth and early metastasis. SCLC is predominantly associated with cigarette smoking, making its occurrence more prevalent in heavy smokers.
Globally, lung cancer is responsible for more fatalities than any other type of cancer, with millions diagnosed each year. In the United States alone, the American Cancer Society estimates over 200,000 new cases annually. The risk factors contributing to the development of lung cancer include smoking, exposure to secondhand smoke, environmental toxins, and genetic predispositions. Furthermore, the increasing rate of lung cancer among non-smokers highlights the importance of understanding this disease comprehensively.
Given the complexity and severity of lung cancer, early detection and treatment are crucial for improving survival rates. Awareness of its symptoms, causes, and types can significantly aid in combating this widespread health issue. As research continues to evolve, advancements in medical technology and targeted therapies hold promise for more effective treatment options in the near future.
Causes and Risk Factors
Lung cancer is influenced by various factors, which can be broadly categorized into modifiable and non-modifiable risks. A predominant cause of lung cancer is exposure to tobacco smoke, which accounts for approximately 85% of all lung cancer cases. Both active smoking and passive exposure significantly elevate the risk, as carcinogens found in tobacco smoke lead to mutations in lung cells. Furthermore, the intensity and duration of smoking habits correlate directly to the likelihood of developing this disease.
In addition to smoking, environmental exposures play a crucial role in lung cancer risk. Air pollution, characterized by fine particulate matter, has been shown to increase the probability of lung cancer, especially in urban areas. Other harmful substances, such as radon gas, can accumulate in homes and buildings, contributing to lung cancer risk as well. Exposure to asbestos—a naturally occurring mineral—is another significant factor, particularly in occupational settings, where workers may inhale fibers that lead to serious lung diseases, including lung cancer.
Genetic predispositions also contribute to lung cancer risk, making some individuals more susceptible to the effects of environmental carcinogens. Certain inherited gene mutations can reduce the body’s ability to repair DNA damage, increasing the likelihood of tumor development. Moreover, familial history of lung cancer may suggest an inherited vulnerability that can augment risk, although the exact mechanisms remain an ongoing area of research.
Occupational hazards are pertinent to specific industries, such as construction or mining, where exposure to certain chemicals and minerals is prevalent. Regular exposure to substances like diesel exhaust, arsenic, or chromium compounds can elevate lung cancer risks among workers. Understanding these causes and risk factors aids in the development of effective prevention strategies and early detection efforts, ultimately contributing to better outcomes in lung cancer management.
Symptoms of Lung Cancer
Lung cancer is a serious health condition that often presents with a range of symptoms, which can vary in severity and may develop gradually over time. One of the most common respiratory symptoms is a persistent cough. Unlike a typical cough that resolves within a few weeks, a cough associated with lung cancer may be chronic and may worsen over time. This cough could also produce blood, which is a concerning sign that warrants medical attention.
Chest pain is another significant symptom that many individuals experience. This pain can manifest as a dull ache or a sharp, stabbing sensation, often worsening with deep breathing, coughing, or laughing. The presence of chest pain can indicate the tumor’s proximity to the chest wall or its impact on surrounding structures. It’s essential for individuals experiencing unexplained chest discomfort to seek evaluation from a healthcare professional, as this symptom can relate to the progression of lung cancer.
Breathlessness, medically known as dyspnea, is also a critical symptom. It may arise due to the obstruction caused by tumors within the airways, leading to labored or difficult breathing. This symptom may emerge gradually and might make physical activities increasingly challenging. Weight loss, particularly when not intentional, can also be a hallmark of lung cancer. This unintentional weight loss may be attributed to the body’s increased metabolic demands in fighting cancer and can lead to a noticeable decline in overall health.
Early detection is paramount in improving outcomes for lung cancer patients. Recognizing these symptoms in their initial stages and seeking prompt medical evaluation can potentially lead to timely interventions, enhancing the likelihood of successful treatment and better quality of life. Being aware of these signs is crucial for individuals, especially those with risk factors, to advocate for their health actively.

Diagnosis of Lung Cancer
Lung cancer diagnosis involves a combination of imaging tests, biopsies, and sometimes molecular testing to ascertain the presence of cancerous cells within the lung tissue. The initial step typically involves imaging techniques such as chest X-rays and computed tomography (CT) scans. These imaging modalities are instrumental in identifying abnormal growths or nodules in the lungs, which may raise suspicion for lung cancer. While chest X-rays provide a basic overview, CT scans offer a more detailed view, allowing for better assessment of the size, shape, and location of any detected abnormalities.
If imaging tests suggest the possibility of lung cancer, a biopsy is generally warranted for a definitive diagnosis. During a biopsy, a small sample of lung tissue is extracted and examined for cancerous cells. Various techniques, including bronchoscopy, needle biopsy, or surgical biopsy, may be employed depending on the location of the anomaly and the patient’s overall condition. The pathology results from the biopsy confirm whether lung cancer is present and provide information on the type of cancer, which is critical for developing an appropriate treatment strategy.
Moreover, understanding the stage of lung cancer is crucial in guiding treatment options. Staging refers to the process of determining how much the cancer has spread within the lungs and to other parts of the body. This information is often gleaned from imaging tests and can significantly impact therapeutic decisions. For example, early-stage lung cancers may be amenable to surgical resection, while advanced stages may require systemic therapies such as chemotherapy or targeted therapies. Additionally, molecular testing may identify specific genetic mutations within the tumor, further informing treatment pathways and tailoring options to the individual patient.
Treatment Options for Lung Cancer
Lung cancer treatment is tailored according to the type, stage, and overall health of the patient. The primary treatment modalities for lung cancer include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Each of these options plays a crucial role in managing the disease and may be employed alone or in combination.
Surgery is often the first line of treatment, especially for non-small cell lung cancer (NSCLC) that is detected early. The goal of surgery is to remove the tumor and any surrounding tissue that may contain cancer cells. Procedures can range from lobectomy, where a lobe of the lung is removed, to pneumonectomy, which involves removing an entire lung. However, not all patients are candidates for surgery, particularly those with advanced disease or compromised health.
Chemotherapy utilizes powerful drugs to target and kill rapidly dividing cancer cells. This treatment is commonly indicated for patients with small cell lung cancer (SCLC) and is often administered after surgery to eliminate residual cancer cells or as a primary treatment for advanced stages. While chemotherapy can be effective, it is associated with several side effects, including nausea, fatigue, and increased risk of infection due to its impact on the immune system.
Radiation therapy employs high-energy beams to target tumors, contributing to pain relief and shrinking tumors when surgery is not feasible. It may also be used post-operatively to annihilate any remaining cancerous cells. Although effective, patients may experience fatigue and skin reactions in the treated area.
Targeted therapy and immunotherapy are newer modalities that focus on specific characteristics of cancer cells or enhance the body’s immune response. Targeted therapy is used for NSCLC with specific genetic mutations, while immunotherapy has shown promise in both NSCLC and SCLC. Side effects can vary widely between these therapies but may include immune-related responses and fatigue.
The Role of Clinical Trials
Clinical trials play a pivotal role in advancing our understanding of lung cancer and enhancing treatment options for patients. These carefully structured studies are essential for evaluating new therapies, drug combinations, and diagnostic methods, enabling researchers to uncover innovative solutions that can potentially improve patient outcomes. By participating in clinical trials, individuals contribute to the broader medical community’s efforts to find more effective treatments for lung cancer, while also potentially gaining access to cutting-edge therapies not yet available to the general public.
When a patient considers participating in a clinical trial, it is crucial to understand both the risks and benefits involved. Clinical trials might offer potential therapeutic advantages, including the exploration of new treatments that may outperform standard therapies. Additionally, participants often receive comprehensive medical care throughout the study period, supervised by a dedicated team of health professionals. However, it is important to acknowledge that experimental treatments may not be effective for every participant and could present unforeseen side effects. As such, patients should engage in thorough discussions with their healthcare providers to assess their eligibility and comfort with the trial’s requirements.
The contribution of clinical trials to lung cancer care is immense. They not only facilitate the testing of new drugs but also allow researchers to gather comprehensive data on the efficacy and safety of these treatments. Through these studies, scientists can investigate varying aspects of the disease, such as genetic factors and tumor biology, which can lead to personalized treatment approaches. Furthermore, successful clinical trials can eventually influence treatment guidelines and standards of care, ultimately benefiting a large population of lung cancer patients. By fostering collaboration among researchers, healthcare providers, and patients, clinical trials usher in a new era of hope in the fight against lung cancer.

Living with Lung Cancer
Living with lung cancer presents numerous challenges, both physically and emotionally. Patients often find that coping mechanisms play a crucial role in managing their daily lives. Compounding the physical effects of the illness, psychological stress can emerge, leading to anxiety and depression. Consequently, it is essential for patients to seek robust support systems, which can include counseling services, support groups, and family involvement. These networks can provide not only emotional comfort but also practical advice based on shared experiences.
Palliative care emerges as a pivotal aspect of managing lung cancer. This approach focuses on improving the quality of life for patients by addressing symptoms and side effects associated with the disease and treatment. Palliative care specialists work alongside oncologists to create a comprehensive care plan tailored to individual needs. This might include pain management, addressing shortness of breath, and tackling fatigue effectively. Patients are encouraged to engage in open dialogues with their care teams about distressing symptoms to facilitate appropriate interventions.
In tandem with medical management, lifestyle changes can substantially impact a patient’s well-being. A nutritious diet is fundamental; foods rich in antioxidants, such as fruits and vegetables, can help counteract the effects of cancer treatment and enhance overall health. Additionally, staying hydrated and opting for smaller, frequent meals may also improve appetite, which can be a common issue during treatment phases.
Emotional health resources are equally important. Mindfulness practices, such as meditation and yoga, can provide significant relaxation benefits. Engaging in hobbies and social activities can help distract from the stressors of living with lung cancer, reinforcing the necessity of a holistic approach to care. By implementing these strategies, individuals facing lung cancer can cultivate resilience, ultimately contributing to a higher quality of life.
Future of Lung Cancer Research
The landscape of lung cancer research continues to evolve rapidly, driven by technological advancements and a better understanding of the disease at the molecular level. Ongoing studies are exploring a variety of emerging therapies that aim to improve treatment outcomes and enhance patient quality of life. Among the most promising avenues of research are immunotherapy and targeted therapies. These modalities harness the body’s immune system to fight cancer or specifically target molecular abnormalities associated with lung cancer, allowing for personalized treatment strategies. For instance, checkpoint inhibitors have demonstrated considerable effectiveness in advanced lung cancer cases, yielding significant improvement in survival rates.
Another critical focus area in lung cancer research is genetic research. Scientists are intensifying their efforts to identify specific genetic mutations that contribute to the development and progression of lung cancer. By pinpointing these mutations, researchers can develop targeted drugs that are more effective and potentially less toxic than traditional chemotherapy. This genetic profiling also allows for earlier interventions, turning the spotlight on prevention and novel treatment protocols tailored to individual patients’ genetic makeups.
Moreover, the potential breakthroughs in early detection techniques hold remarkable promise for the future of lung cancer outcomes. Techniques such as liquid biopsy are being refined to detect circulating tumor DNA in the blood, which could revolutionize the way lung cancer is diagnosed and monitored. Such non-invasive methods may facilitate earlier and more accurate diagnoses, ultimately leading to better prognoses for patients. As these advancements in lung cancer research continue to unfold, the medical community remains optimistic about the potential for innovative treatments and improved survival rates, instilling hope for patients diagnosed with this formidable disease.
FAQ: Understanding Lung Cancer
Lung cancer remains a serious health concern globally, prompting many individuals to seek information on various aspects related to the disease. The following FAQ section aims to provide evidence-based answers to common inquiries surrounding lung cancer.
What are the survival rates for lung cancer?
Survival rates for lung cancer can vary based on several factors, including the type of lung cancer, stage at diagnosis, and overall health of the patient. According to the American Cancer Society, the overall five-year survival rate for lung cancer is approximately 20%. However, for localized cases detected early, the survival rate can be as high as 60%. These statistics underscore the importance of early detection and timely treatment.
Does quitting smoking improve lung cancer outcomes?
Yes, smoking cessation can significantly improve outcomes for individuals diagnosed with lung cancer. Studies have shown that quitting smoking can enhance the effectiveness of treatments such as surgery, chemotherapy, and radiation. Furthermore, it may decrease the risk of developing second primary lung cancers, providing added motivation for patients to stop smoking, regardless of their cancer stage.
Is there a chance of lung cancer recurrence after treatment?
The possibility of recurrence depends on various factors, including the cancer type, stage, and treatment methods. Recurrences can happen, particularly within the first two years following treatment. Surveillance through regular follow-up appointments is crucial, as healthcare providers can offer early detection of any returning disease.
Can genetic factors increase lung cancer risk?
Yes, genetic predisposition can play a significant role in lung cancer risk. While smoking is the leading cause, certain individuals may inherit mutations that increase susceptibility to lung cancer. Genetic counseling and testing may be recommended for those with a family history of lung cancer or other related malignancies.
In conclusion, understanding common inquiries related to lung cancer helps demystify the condition and promotes informed decisions concerning prevention, treatment, and support options. By addressing these frequently asked questions, the hope is to provide clarity and empower individuals facing the challenges associated with lung cancer.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

