What is Pectus Excavatum?
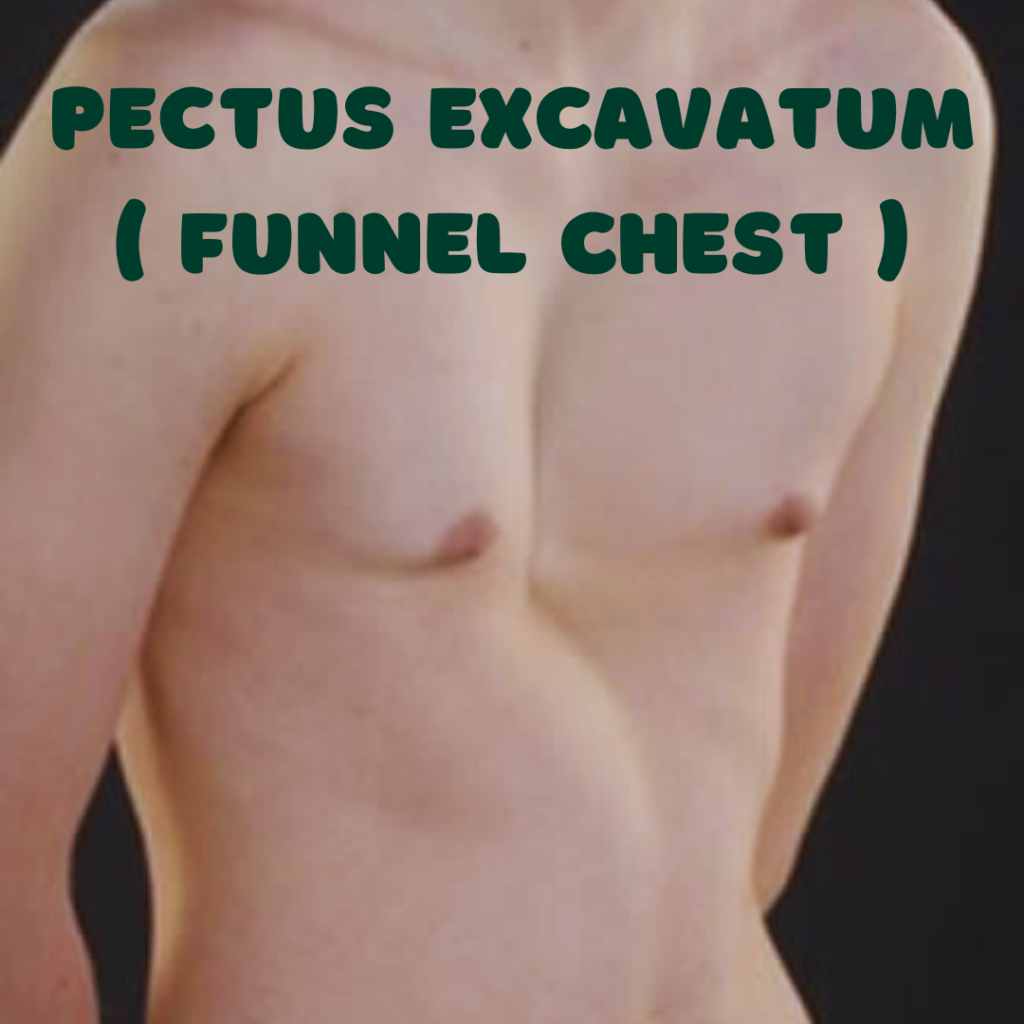
Pectus excavatum, often referred to as “sunken chest” syndrome, is a congenital deformity wherein the sternum and parts of the rib cage are recessed into the chest cavity, causing a noticeable indentation. This condition can vary in severity, with some individuals experiencing only a slight dip in their chest wall while others may have a more pronounced and pronounced appearance. It is one of the most common congenital chest wall deformities, affecting approximately 1 in every 300 to 400 births. While pectus excavatum is typically diagnosed in infancy or childhood, some cases may not become apparent until later in life during adolescence.
The assessment of pectus excavatum typically involves a thorough physical examination, where a physician will observe the chest’s appearance and may request imaging studies, such as a chest X-ray or CT scan, to evaluate the structural aspects of the chest wall and its impact on internal organs. Understanding the condition is crucial not only for those affected but also for their families. With early diagnosis and appropriate management, complications can often be minimized. The condition is associated with various symptoms, ranging from cosmetic concerns to potential respiratory and cardiovascular issues in severe cases.
Pectus excavatum is predominantly a genetic condition, and its origins are not entirely understood. Current research suggests that it may result from abnormal growth patterns of cartilage in the rib cage. Individuals and families affected by pectus excavatum may benefit from learning more about the condition, available treatment options, and potential long-term outcomes. Being informed empowers individuals to make educated decisions regarding their medical care and management strategies.
Anatomy of the Chest
The anatomy of the chest is intricate and plays a crucial role in protecting vital organs and supporting respiratory function. The primary components of the chest include the sternum, ribs, and diaphragm. Understanding how pectus excavatum affects these structures is essential for comprehending the condition and its treatment.
The sternum, commonly referred to as the breastbone, is a flat bone located at the front of the chest. It connects with the ribs through cartilage, forming the ribcage which aids in respiration. In individuals with pectus excavatum, the sternum is abnormally retracted into the chest wall, creating a “caved-in” appearance that can impact both aesthetic and physiological factors. This deformity can lead to limited thoracic capacity, affecting lung function and overall health.
The ribs, twelve pairs in total, are curved bones that form a protective cage around the organs in the thoracic cavity. They articulate with the thoracic vertebrae at the back and connect to the sternum at the front through costal cartilage. In cases of pectus excavatum, the position and orientation of the ribs may also become altered, which can further restrict expansion during inhalation, potentially leading to respiratory issues.
Connecting the ribs and facilitating the movement of air is the diaphragm, a dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm plays an integral role in breathing, and with altered chest anatomy due to pectus excavatum, its function can be compromised. The mechanical stress placed on this muscle may result in reduced efficiency in airflow, further exacerbating the struggle to take deep breaths.
By thoroughly understanding the anatomy of the chest and how pectus excavatum modifies these structures, clinicians and patients alike can better assess the necessity and type of treatment options available. The awareness of how these components interact is vital in managing the condition effectively.
Causes and Risk Factors
Pectus excavatum, characterized by an inward depression of the sternum, is a congenital condition that may arise from a combination of genetic and environmental influences. One of the leading hypotheses regarding its etiology is related to genetic predisposition. Family history plays a significant role, as conditions such as Marfan syndrome and Ehlers-Danlos syndrome, known for their connective tissue abnormalities, often present alongside cases of pectus excavatum. The heritability of this condition highlights the possibility of a genetic component wherein certain variants can lead to a structural deficiency in the chest wall.
Collagen abnormalities are also critical in the development of pectus excavatum. Connective tissue disorders can weaken the structural integrity of the chest wall, leading to the characteristic indentation. Recent studies have revealed that improper collagen synthesis can cause the ribs and sternum to grow in a manner that favors this deformity. Variations in collagen type and structure may disrupt normal growth patterns, resulting in the underdevelopment of anterior thoracic structures.
Furthermore, environmental factors may contribute as well, albeit less directly. For instance, certain lifestyle behaviors during childhood, such as poor posture or lack of physical activity, may exacerbate the degree of the chest wall deformity, particularly in susceptible individuals. Interestingly, recent research suggests that respiratory health during critical growth periods may impact the progression of pectus excavatum, placing additional emphasis on understanding how external factors can interact with underlying genetic risks.
In summary, the interplay of genetic predispositions, collagen abnormalities, and certain lifestyle factors underscores the complexity of pectus excavatum. Understanding these causes and risk factors plays an essential role in diagnosing and managing this condition effectively.

Signs and Symptoms
Pectus excavatum, often characterized as a funnel chest, is a congenital deformity resulting in a depression of the sternum, leading to various physical manifestations. Individuals with this condition typically exhibit noticeable alterations in posture and overall chest shape. The most apparent sign is the inward curvature of the breastbone, which becomes pronounced when the individual is standing or sitting upright. This deformity may vary in severity, influencing the degree to which the chest appears ‘sunken’ and the individual’s overall physical presentation.
Alongside these visible signs, pectus excavatum can also give rise to potential respiratory issues. The altered chest structure may restrict lung expansion, leading to decreased lung capacity and, consequently, reduced oxygenation of the blood. Individuals may experience difficulties during physical activities, often reporting shortness of breath, especially when engaging in strenuous exercise. Furthermore, this impaired respiratory function can contribute to fatigue and diminished overall stamina, negatively affecting the quality of life.
Psychological impacts are another significant aspect associated with pectus excavatum. Adolescents and young adults with this condition may experience social anxiety, body image issues, or lowered self-esteem due to their physical appearance. Often, this can lead to withdrawal from social activities, further exacerbating feelings of isolation or discomfort in social settings. It is essential to recognize the holistic implications of pectus excavatum, as both physical and psychological symptoms can intersect, influencing the individual’s well-being. Understanding these signs and symptoms can help parents and individuals identify whether they may be affected by this condition, fostering awareness and encouraging timely medical consultation when necessary.
Diagnostic Procedures
Pectus excavatum is a structural deformity characterized by a sunken appearance of the chest. Accurate diagnosis is essential for determining the most effective treatment options for individuals affected by this condition. The diagnostic process typically begins with a thorough physical examination performed by a qualified healthcare professional, who assesses the chest shape and may inquire about any associated symptoms such as shortness of breath or chest pain.
Following the physical assessment, various imaging techniques play a crucial role in confirming the diagnosis of pectus excavatum. One commonly used method is the chest X-ray. This imaging procedure provides a basic overview of the chest anatomy and can help identify the degree of the deformity. However, while chest X-rays are useful, they may not provide complete information on the severity of the condition or potential complications.
For a more detailed examination, healthcare providers often recommend a computed tomography (CT) scan. CT imaging offers a comprehensive view of the chest structures, allowing for precise measurements of the chest’s depth and width. Additionally, it can reveal any impact on the heart and lungs, which is vital for assessing how pectus excavatum may affect respiratory and cardiovascular function. The CT scan can help determine the best course of action, particularly when surgical interventions are considered.
It is clear that a thorough diagnostic process is imperative for effective management of pectus excavatum. By utilizing a combination of physical exams and advanced imaging techniques, healthcare professionals can accurately assess the condition and tailor treatment approaches accordingly. Early diagnosis and intervention can significantly improve quality of life for those affected by this deformity.
Treatment Options
Pectus excavatum presents various treatment options that cater to different severity levels and patient preferences. Understanding these options is crucial for patients and their families in making informed decisions. Treatment generally falls into two categories: non-surgical and surgical methods.
Non-surgical approaches often serve as initial interventions, particularly for mild cases. Physical therapy is one prominent option, focusing on exercises designed to improve posture and strengthen the chest muscles. This method can enhance the appearance of the chest and alleviate some functional issues, often without the need for surgical intervention. Additionally, braces may be used, especially in younger patients whose chests are still developing. Bracing aims to push the ribcage outward, encouraging a more typical chest contour over time. While these non-invasive methods may not provide significant correction for severe cases, they can be beneficial for mild instances and generally carry fewer risks.
When non-surgical methods are insufficient, surgical interventions become relevant. The Nuss procedure, which involves the insertion of a curved metal bar beneath the sternum, is a minimally invasive technique designed for patients with moderate to severe pectus excavatum. This method has the advantage of a shorter recovery time compared to traditional surgery, but it does come with potential risks, such as infection or bar displacement. Conversely, the Ravitch procedure is more invasive and includes the removal of any abnormal cartilage and the repositioning of the sternum. While this method can offer significant corrective results, it involves a longer recovery period and higher risks.
The choice of treatment should depend on individual circumstances, including the severity of the condition, the patient’s age, and overall health. Consulting with a healthcare professional specializing in pectus excavatum is essential to determine the most suitable option tailored to each individual.

Living with Pectus Excavatum
Living with pectus excavatum can pose unique challenges, both physically and emotionally. Individuals diagnosed with this condition often experience a range of symptoms, including reduced exercise tolerance and potential respiratory issues, which can impact daily life. One of the most crucial aspects of managing pectus excavatum is engaging in coping strategies that can enhance one’s quality of life. Openly discussing feelings and concerns with family and friends can provide emotional support, while engaging in regular physical activity can help in maintaining overall health and improving confidence.
Forming or joining support groups can be incredibly beneficial. These gatherings allow individuals with pectus excavatum to share experiences, tips, and strategies for coping with the condition. Such communities foster a sense of belonging and reduce feelings of isolation. Furthermore, these interactions can provide insights from those who have successfully navigated challenges associated with pectus excavatum, offering a wealth of knowledge and practical advice for newcomers who may feel overwhelmed.
Mental health is an often-overlooked aspect of living with pectus excavatum. Individuals may experience anxiety or depression linked to body image issues or physical limitations that arise from the condition. It is vital to recognize these feelings and seek professional help when necessary. Counseling or therapy can provide tools to build resilience and enhance coping mechanisms. Self-advocacy is essential; individuals should feel empowered to communicate their health needs and seek assistance, whether from healthcare providers or support networks.
Finally, maintaining an active lifestyle is important for managing pectus excavatum. Engaging in low-impact exercises, such as swimming or yoga, can contribute positively to physical condition and mental well-being. Encouraging healthy habits can lead to a more fulfilling life despite the challenges posed by pectus excavatum. Support, understanding, and proactive engagement are key to successfully navigating the journey with this condition.
FAQs about Pectus Excavatum
Pectus excavatum is a condition that raises many questions due to its complexity and the effects it can have on individuals. Below are some frequently asked questions regarding this condition to provide clarity and guidance for those affected.
What are the long-term effects of pectus excavatum?
Long-term effects of pectus excavatum can vary significantly among individuals. In some cases, the condition may be purely cosmetic, causing no substantial health issues. However, for others, especially severe cases, it can impact lung and heart function over time. As the chest cavity becomes more compressed, it might lead to respiratory issues or reduced exercise tolerance. Early detection and treatment can mitigate these potential complications.
Does pectus excavatum impact physical activity?
Many individuals with pectus excavatum continue to participate in regular physical activity. However, those with more severe forms may experience limitations due to symptoms such as shortness of breath or reduced stamina. Engaging in low-impact activities initially and gradually increasing intensity can help in maintaining fitness levels. It is crucial to consult a healthcare provider to tailor an exercise plan suited to individual capabilities and comfort levels.
Can pectus excavatum worsen with age?
Pectus excavatum can indeed progress as individuals age, particularly during periods of rapid growth in adolescence. As the chest wall continues to develop, the severity of the indentation may become more pronounced. Regular monitoring by a healthcare professional is advisable to assess any changes and to determine if treatment interventions may be necessary.
What should parents consider if their child has pectus excavatum?
Parents should consider the implications of pectus excavatum on their child’s physical and emotional well-being. While some children may not experience significant effects, others might face social anxiety or reduced self-esteem related to their appearance. Observing your child’s physical activity levels and overall confidence can help in deciding whether a consultation with a specialist is needed. Early intervention can lead to better long-term outcomes, both physically and psychologically.
Conclusion and Resources
In conclusion, understanding pectus excavatum is crucial for those affected by this condition, as well as for their families and friends. Pectus excavatum, characterized by a sunken appearance of the chest, can lead to both physical and emotional challenges. Awareness of its causes, such as genetic factors and developmental issues, along with the various symptoms—including respiratory and cardiovascular difficulties—enhances our ability to address this condition effectively. Recognizing the symptoms early can facilitate timely intervention and improve overall quality of life.
While treatment options vary depending on the severity of the condition, there are several effective approaches available, ranging from monitoring and physical therapy to surgical options for more pronounced cases. Engaging with healthcare professionals who specialize in pectus excavatum can provide invaluable guidance for both patients and their families as they navigate the complexities of this condition.
To further enhance knowledge and support for individuals dealing with pectus excavatum, a curated list of resources is available. Support groups can offer a community of shared experiences, providing emotional comfort and practical advice. Articles from reputable medical journals and organizations underscore important research findings and give insights into innovative treatment methods. Consulting with specialized healthcare professionals—such as thoracic surgeons, pediatricians, or physical therapists—ensures that patients receive tailored care and the best treatment options available.
Ultimately, fostering an understanding of pectus excavatum empowers individuals and their support networks, facilitating a proactive approach to managing this condition. Knowledge is a powerful tool for patients seeking to lead healthy, fulfilling lives despite the challenges posed by pectus excavatum.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

