Seizures and the Nervous System : 7 Shocking Facts
Seizures and the Nervous System
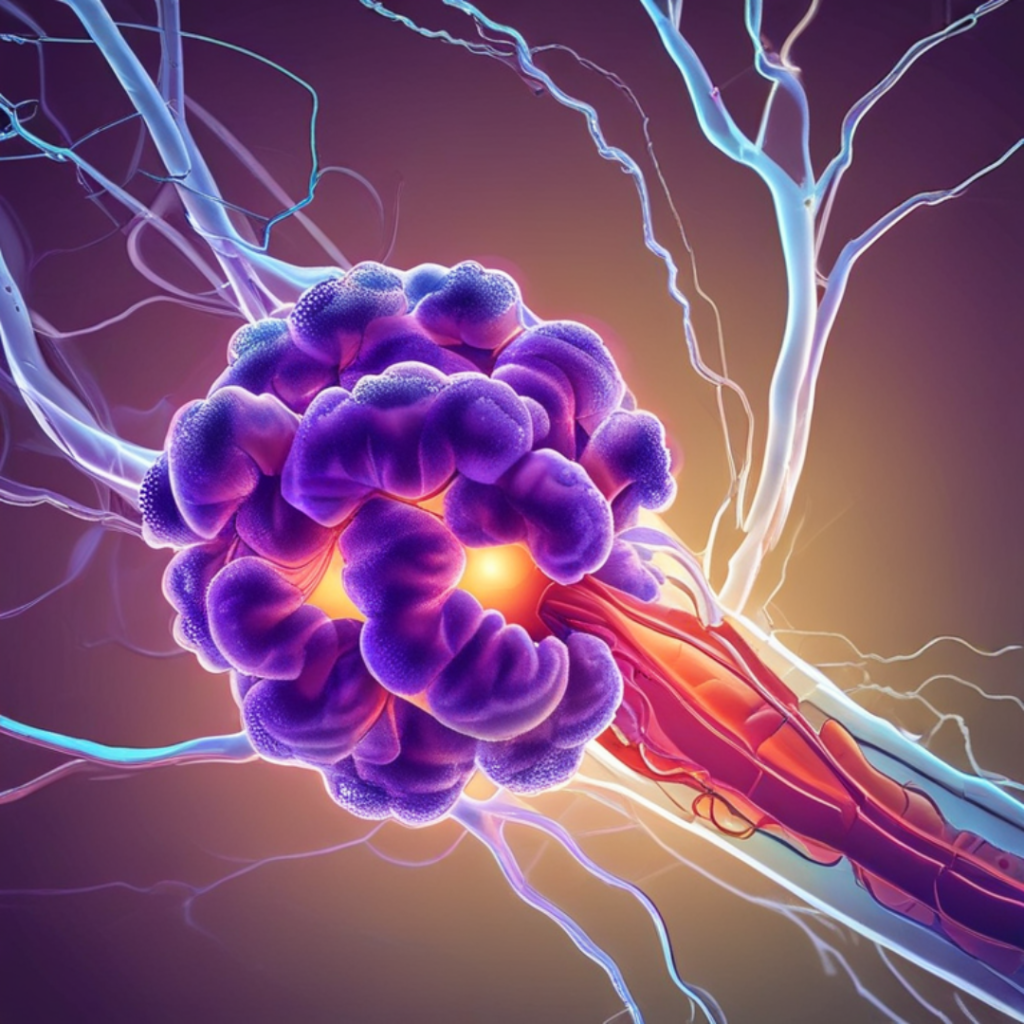
Seizures are complex neurological events characterized by sudden, uncontrolled electrical disturbances in the brain. Understanding seizures requires a fundamental grasp of the nervous system’s anatomy and function. The nervous system, composed of the brain, spinal cord, and a vast network of neurons, serves as the body’s communication infrastructure, transmitting signals that control various bodily functions.
Sign up for HUMANITYUAPD
At the core of this network are neurons, specialized cells responsible for conveying electrical impulses. These impulses, or action potentials, facilitate communication between different regions of the nervous system. When these electrical signals are disrupted, as is the case during a seizure, the result can be varied, ranging from mild, momentary lapses in awareness to severe, convulsive episodes.
Seizures can be triggered by numerous factors, including genetic predispositions, brain injuries, infections, and certain medical conditions such as epilepsy. The precise cause of a seizure often influences its type and severity. For instance, focal seizures originate in a specific area of the brain and might only affect that region’s function. In contrast, generalized seizures involve multiple areas of the brain from the onset, often leading to more widespread symptoms.
Electrophysiological disturbances within the brain’s neural pathways play a crucial role in seizure activity. These disturbances may result from abnormal synaptic transmission, ion channel dysfunctions, or imbalances in neurotransmitters, which are chemicals that facilitate neuron communication. During a seizure, these disruptions manifest as erratic electrical discharges that can temporarily alter brain function.
Comprehending the intricate relationship between neurons and electrical activity within the brain is essential for understanding seizures. This foundation facilitates a deeper exploration into the diagnosis, treatment, and management of seizure disorders, while underscoring the importance of ongoing research in the field of neurology. The nervous system’s complexity highlights the need for a detailed, nuanced approach to studying seizures, ensuring better outcomes for those affected by these challenging neurological events.
➡️ Table of Contents ⬇️
Types of Seizures and Their Symptoms
Seizures are complex neurological events with diverse manifestations, distinguishing them into several types based on their origin and symptoms. Primarily, seizures are categorized into focal (partial) seizures, generalized seizures, and unknown onset seizures. These classifications enable better understanding and management of seizure disorders.
Focal Seizures: Also known as partial seizures, focal seizures originate in a specific area of the brain. They are further divided into simple focal seizures, where consciousness is not impaired, and complex focal seizures, which affect consciousness or awareness. Symptoms of simple focal seizures may include involuntary muscle jerking, sensory changes such as tingling or hallucinations, and emotional variations. Complex focal seizures, however, may involve altered consciousness, automatisms like lip-smacking, and an aura—a perceptual disturbance experienced before the actual seizure.
Generalized Seizures: These seizures affect both hemispheres of the brain simultaneously. Among the various types, the most commonly observed are tonic-clonic (grand mal) seizures, which involve stiffening (tonic phase) followed by rhythmic jerking of muscles (clonic phase). Other generalized seizures include absence seizures, characterized by brief lapses in awareness, often mistaken for daydreaming, and atonic seizures, which cause sudden loss of muscle tone leading to falls. Myoclonic seizures and tonic seizures also fall under this category, manifesting as quick muscle jerks and sudden muscle stiffening, respectively.
Unknown Onset Seizures: When the onset of a seizure is not observed or recorded, it is classified as an unknown onset seizure. Over time, as more information becomes available, an unknown onset seizure may be reclassified as either focal or generalized. Recognizing the symptoms, such as sudden onset of altered behavior, convulsions, or muscle rigidity, is crucial in diagnosing and managing these seizures accurately.
Understanding the types of seizures and their presenting symptoms is critical for timely medical intervention and effective treatment. Watching for signs such as unusual muscle movements, changes in sensation or behavior, and conscious disturbances can aid in identifying seizures and seeking appropriate care.
Diagnosis and Mapping of Seizures
Accurately diagnosing seizures involves a comprehensive approach to ensure appropriate treatment and management. Medical professionals typically begin with a detailed neurological examination to assess brain function, identifying any abnormalities that may signal seizure activity. This examination often includes tests of reflexes, muscle tone, and sensory response to thoroughly evaluate the nervous system’s integrity.
Following the neurological exam, imaging tests such as magnetic resonance imaging (MRI) and computed tomography (CT) scans are commonly employed. These advanced imaging modalities offer detailed views of the brain’s structure, allowing doctors to detect lesions, tumors, or other abnormalities that could be related to seizures. MRI is particularly useful for spotting structural issues not visible on CT scans, providing a higher resolution and greater detail.
An essential tool in seizure diagnosis is the electroencephalogram (EEG). By measuring electrical activity in the brain through electrodes placed on the scalp, the EEG can identify abnormal patterns indicative of seizures. This non-invasive test records brain wave patterns over a period, which can be analyzed for irregularities suggesting epilepsy or other seizure disorders. Sometimes, a prolonged EEG monitoring, known as an ambulatory EEG, is necessary to capture seizure activity that doesn’t occur during a short test period.
Mapping seizures is a crucial process that enhances understanding of their origins and pathways within the brain. Specialists analyze the data gathered from EEGs alongside imaging results to pinpoint which areas of the brain are involved in seizure activity. This mapping process is vital for formulating targeted treatment plans, particularly for patients who require surgical interventions. Identifying specific regions affected by seizures allows neurosurgeons to plan precise surgical procedures aimed at reducing or eliminating seizure episodes while preserving essential brain functions.
Overall, the diagnosis and mapping of seizures represent a multidisciplinary effort, combining clinical expertise, advanced imaging technologies, and precise electrical monitoring. Through this integrative approach, medical professionals can provide tailored treatment options that significantly improve the quality of life for individuals suffering from seizure disorders.

Treatment Options and Management Strategies
Managing seizures effectively requires a comprehensive approach that often combines multiple treatment options. Medication is typically the first line of treatment for individuals diagnosed with seizure disorders. Antiepileptic drugs (AEDs) are designed to reduce the frequency and severity of seizures. The choice of medication depends on various factors, including the type of seizure, patient age, and potential side effects. Some common AEDs include carbamazepine, valproate, and lamotrigine. Importantly, medication regimens need to be closely monitored and adjusted by healthcare professionals to ensure optimal efficacy and minimal side effects.
In addition to medications, lifestyle changes play a crucial role in seizure management. Patients are often advised to avoid known seizure triggers, such as specific foods, stress, and certain activities. Regular exercise, a balanced diet, and adequate sleep can also help in stabilizing the nervous system and reducing seizure episodes. Stress management techniques, including yoga, meditation, and cognitive-behavioral therapy, are often recommended to help patients manage anxiety, which can be a prevalent trigger for many.
For some individuals, surgical interventions may be necessary when medications and lifestyle modifications are insufficient. Procedures like lobectomy, corpus callosotomy, or vagus nerve stimulation (VNS) can be considered. Surgery aims to either remove the area of the brain where seizures originate or to interrupt the neural pathways through which seizure impulses travel. However, surgical options are typically reserved for those who do not respond well to other treatments and require a thorough evaluation by a specialized medical team.
Alternative therapies are also part of a holistic approach to seizure management. Techniques such as acupuncture, ketogenic diets, and CBD (cannabidiol) oils have shown promise for some patients, though scientific evidence supporting their efficacy varies. It is essential for patients considering these options to consult with their healthcare team to ensure safety and compatibility with their established treatment plan.
The cornerstone of effective seizure management is a personalized treatment plan that considers the unique needs of each patient. Continuous monitoring and regular follow-ups with healthcare providers are critical to adapting treatment strategies over time. This personalized and dynamic approach ensures that the management plan evolves as the patient’s condition and circumstances change.
Living with Seizures: Tips and Recommendations
Living with seizures poses unique challenges that require practical strategies to manage effectively. One of the first steps in managing the condition is identifying and avoiding potential triggers. Common triggers include stress, lack of sleep, flashing lights, and certain foods or beverages. Keeping a seizure diary can be instrumental in tracking these triggers, helping individuals pinpoint patterns that should be avoided to minimize the risk of seizures.
Safety precautions play a crucial role in living with seizures. Simple modifications such as installing safety guards around sharp edges, using non-slip mats, and ensuring a clutter-free environment can significantly reduce the risk of injury during a seizure. Additionally, wearing a medical alert bracelet can provide quick identification and necessary information to first responders, ensuring prompt and appropriate care during an emergency.
Engaging in certain lifestyle modifications can also make a considerable difference. A balanced diet, regular exercise, and maintaining a consistent sleep schedule contribute to overall well-being and can help stabilize seizure activity. Equally important is adhering to prescribed medication regimens and attending regular medical appointments to monitor the condition closely.
Support systems are indispensable for individuals living with seizures. Family, friends, and support groups can provide not only emotional solace but also practical assistance. Participating in support groups fosters a sense of community where experiences and coping strategies are shared, alleviating feelings of isolation.
Mental health considerations are another pivotal aspect of managing seizures. The unpredictability of seizure occurrences can lead to anxiety, depression, and social withdrawal. Therefore, seeking professional mental health support and possibly integrating therapies such as cognitive-behavioral therapy (CBT) can provide valuable tools for coping with these challenges.
Maintaining a high quality of life despite the condition is attainable with mindfulness, preparation, and a robust support system. By implementing these tips and recommendations, individuals can navigate the complexities of living with seizures more confidently and effectively.
The Role of Technology in Seizure Management
Seizure management has witnessed significant strides thanks to the integration of innovative technologies. These advancements are transforming the approach to monitoring, detecting, and treating seizures, thereby offering enhanced care for individuals affected by epilepsy and other neurological disorders.
One of the most notable innovations is the advent of wearable devices designed specifically for seizure monitoring. These devices, which often take the form of wristbands or patches, continuously track physiological parameters such as heart rate, muscle activity, and skin conductance. When abnormal patterns indicative of a seizure are detected, the device can alert caregivers or medical professionals immediately, ensuring swift intervention.
Furthermore, seizure detection apps have emerged as powerful tools in managing epilepsy. Utilizing machine learning algorithms, these apps analyze data from wearable devices, smartphones, or other connected health technologies to predict seizures before they occur. Such predictive capabilities not only offer individuals greater control over their condition but also contribute to personalized treatment plans by providing detailed insights into seizure patterns and triggers.
Advancements in neuroimaging are also playing a pivotal role in understanding and managing seizures. High-resolution imaging techniques like functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) scans allow neurologists to visualize the brain’s activity in unprecedented detail. By identifying specific brain regions involved in seizure activity, these technologies enable precise and targeted interventions, ranging from medication adjustments to surgical planning.
Moreover, the integration of machine learning has opened new horizons in seizure management. By analyzing vast datasets of neuroimaging and electrophysiological recordings, machine learning models can identify subtle patterns that may be overlooked by human analysis. This has the potential to uncover novel biomarkers for epilepsy, leading to earlier diagnosis and more effective treatments.
Collectively, these technological advancements are revolutionizing the landscape of seizure management. By leveraging wearable technology, sophisticated mobile apps, cutting-edge neuroimaging techniques, and machine learning, healthcare providers are better equipped to understand, predict, and treat seizures, ultimately improving the quality of life for individuals affected by these challenging conditions.

Research and Future Directions in Seizure Studies
Emerging research in neurology continues to expand our understanding of seizures and opens up new avenues for treatment and management. One of the key areas of focus is the identification of biomarkers that can predict the onset of seizures. These biomarkers, found through sophisticated genetic and neuroimaging techniques, offer the potential for preemptive intervention, reducing the frequency and severity of seizures.
Additionally, the exploration of neurostimulation therapies has shown considerable promise. Techniques such as transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS) are being refined to target specific areas of the brain involved in seizure activity. Initial studies suggest these methods can significantly reduce seizure occurrences and improve the quality of life for individuals with refractory epilepsy.
Another innovative area of research is the development of seizure prediction algorithms. Using advanced machine learning models, researchers aim to analyze EEG data in real-time to forecast seizure events. These predictive algorithms could lead to the creation of wearable devices, giving patients and caregivers critical alerts to manage seizures proactively. This progression towards personalized medicine marks a substantial leap forward in seizure management.
Moreover, ongoing genetic research is shedding light on the hereditary aspects of seizure disorders. By identifying specific genetic mutations linked to epilepsy, scientists are working towards gene therapy solutions that could correct these anomalies at the molecular level. Such targeted treatments could potentially offer cures for certain forms of epilepsy, pushing the boundaries of what is currently possible in neuroscience.
Finally, pharmaceutical advancements remain a cornerstone of seizure studies. Researchers are continually exploring new compounds and drug combinations to improve therapeutic outcomes for epilepsy patients. The focus is not only on efficacy but also on minimizing side effects, ensuring safer long-term management of seizure disorders.
The future of seizure research holds immense promise as interdisciplinary collaborations, technological advancements, and innovative treatments converge. These efforts are fundamental to transforming our approach to understanding and ultimately curing seizure disorders.
Frequently Asked Questions (FAQs)
Seizures can be a bewildering and distressing experience, both for the individual affected and their loved ones. To provide some clarity, we have compiled answers to some frequently asked questions about seizures and the nervous system.
What triggers a seizure?
Seizures can be caused by a variety of factors including brain injury, infections, genetic predispositions, high fever in children, or even metabolic disturbances. In some cases, the exact trigger remains unknown. It is essential to consult with a healthcare provider for a thorough evaluation.
What are the common symptoms of a seizure?
Seizure symptoms can vary significantly. They range from sudden, uncontrolled jerking movements and loss of consciousness to subtle signs like staring spells, lip-smacking, or confusion. Identifying the type of seizure is crucial for appropriate treatment and management.
How are seizures diagnosed?
Diagnosis usually involves a comprehensive neurological examination, medical history review, and diagnostic tests such as an electroencephalogram (EEG) or brain imaging studies like MRI or CT scans. These tests help determine the underlying cause and guide treatment decisions.
What treatment options are available for seizures?
Treatment typically includes antiepileptic medications to control seizure activity. For some individuals, surgical interventions, dietary modifications like the ketogenic diet, or neurostimulation therapies might be recommended. A tailored treatment plan is essential, often developed in consultation with a neurologist.
How can one manage seizures in daily life?
Managing seizures involves medication adherence, regular medical check-ups, and lifestyle adjustments such as adequate sleep, stress management, and avoidance of known triggers. Education and support for both patients and caregivers play a crucial role in effective management.
What is the prognosis for someone with seizures?
The prognosis varies depending on the underlying cause, type of seizures, and responsiveness to treatment. While some individuals achieve complete seizure control, others might experience persistent episodes. Ongoing medical care and support are vital for improving quality of life.
Can stress cause seizures?
Yes, stress can be a potential trigger for seizures in some individuals, especially those with epilepsy. Stress-related hormonal changes and its effects on the brain’s electrical activity may increase the likelihood of seizures. Learning stress management techniques like mindfulness or relaxation exercises can help reduce this risk.
Are seizures always linked to epilepsy?
No, not all seizures are related to epilepsy. Single or isolated seizures can occur due to factors like fever (febrile seizures), head injuries, infections, or withdrawal from certain substances. Epilepsy is diagnosed when an individual experiences recurrent, unprovoked seizures.
Can someone with seizures live a normal life?
Many individuals with seizures lead normal, fulfilling lives with appropriate treatment and management. Following medical advice, avoiding known triggers, and staying informed about their condition can help maintain an active and balanced lifestyle.
Are seizures hereditary?
Genetics can play a role in some types of epilepsy or seizure disorders, but not all seizures are hereditary. A family history may increase the likelihood of seizures in certain cases, but environmental and medical factors also contribute significantly.
Can seizures be prevented?
Preventing seizures may be possible by addressing underlying causes or triggers. For example, treating infections promptly, maintaining a healthy lifestyle, and taking prescribed medications as directed can reduce the risk. Avoiding alcohol or sleep deprivation can also help prevent seizures in susceptible individuals.
Is it safe for someone with seizures to drive?
Driving regulations vary depending on local laws and the individual’s seizure control status. In most cases, individuals with uncontrolled seizures are advised not to drive. A seizure-free period, verified by a healthcare provider, is typically required before driving privileges are restored.
What should I do if I witness someone having a seizure?
If you witness someone having a seizure:
- Stay calm and ensure the person is in a safe place, away from hazards.
- Turn them gently onto their side to prevent choking.
- Do not place anything in their mouth.
- Time the seizure and seek medical help if it lasts longer than 5 minutes or if it is their first seizure.
Can seizures cause long-term damage?
The potential for long-term damage depends on the type and severity of the seizure. Prolonged or repeated seizures without recovery (status epilepticus) can lead to brain damage. However, most seizures, when managed properly, do not cause lasting harm.
Are there alternative therapies for managing seizures?
In addition to conventional treatments, alternative approaches such as biofeedback, acupuncture, or yoga may help some individuals manage seizures. However, these should complement, not replace, standard medical treatments and be discussed with a healthcare provider.
Can seizures happen during sleep?
Yes, seizures can occur during sleep and are known as nocturnal seizures. These may manifest as unusual movements, noises, or confusion upon waking. Proper diagnosis and treatment are crucial to prevent complications like sleep disruption or injuries.
We hope these answers help address the most pressing concerns about seizures and the nervous system, offering a foundation for better understanding and management of this condition.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

