Hyperpigmentation: 5 Effective Solutions to Try
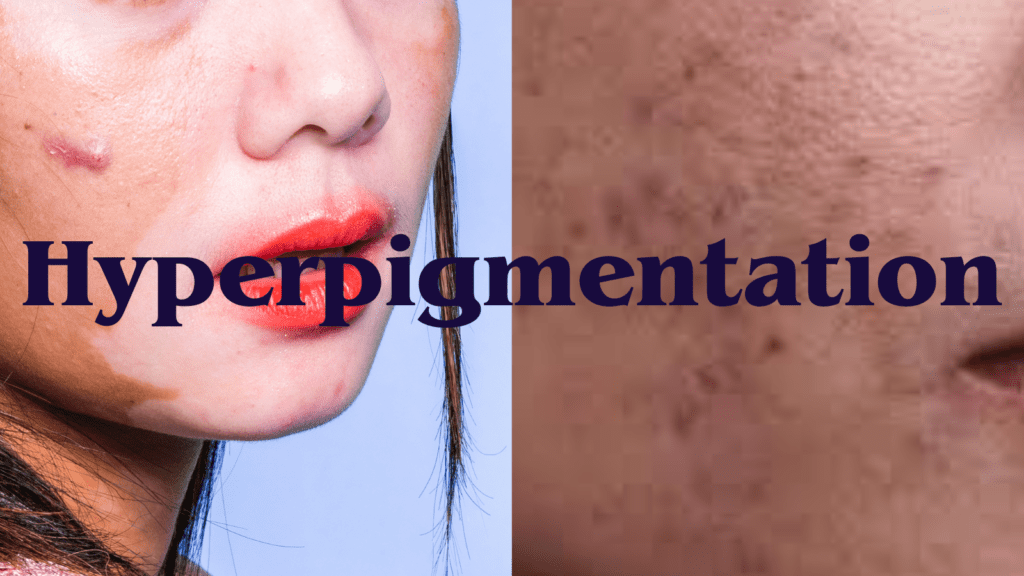
What is Hyperpigmentation?
Hyperpigmentation is a prevalent skin condition characterized by the darkening of specific areas of the skin due to excess production of melanin, the pigment responsible for skin color. This condition manifests itself in various forms, often resulting in uneven skin tone and different shades on the surface. While it is generally harmless, hyperpigmentation can be a cosmetic concern for many individuals, prompting a desire for effective treatment options.
There are several types of hyperpigmentation, with some of the most common being solar lentigines and post-inflammatory hyperpigmentation (PIH). Solar lentigines, often referred to as sunspots or liver spots, arise due to long-term exposure to ultraviolet (UV) light. They are typically larger, flat patches found on sun-exposed areas of the body, such as the face, hands, and arms. As a result, individuals who spend significant time outdoors without adequate sun protection may experience an accelerated formation of these dark spots.
Another prevalent type is post-inflammatory hyperpigmentation, commonly known as PIH. This form occurs following an injury or inflammation to the skin, such as acne, eczema, or psoriasis. After the healing process, affected areas may become darker than the surrounding skin, leading to a disparity in skin tone. PIH can affect individuals of all skin types and tends to be more prominent in people with darker skin tones.
Understanding the various forms of hyperpigmentation is crucial for those seeking ways to address their skin concerns. Identifying the underlying cause is key to determining the most effective treatment path, whether it be through topical applications, professional treatments, or preventive measures.
Causes of Hyperpigmentation
Hyperpigmentation is a complex skin condition that arises from various factors, leading to uneven skin tone and darkened areas on the skin’s surface. One of the primary causes of hyperpigmentation is excessive sun exposure. Ultraviolet (UV) rays stimulate melanocytes, the cells that produce melanin, resulting in increased pigmentation. When the skin is chronically exposed to sunlight without proper protection, it can lead to solar lentigines, commonly known as sun spots.
Hormonal changes also play a significant role in the development of hyperpigmentation. A notable example is melasma, which is often triggered by hormonal fluctuations during pregnancy or with the use of contraceptives. Melasma presents as brown patches predominantly on the face, indicating a direct relationship between hormones and pigmentation changes.
Aging is another contributing factor. As the skin matures, the natural turnover of skin cells slows down, and melanin production can become uneven. This leads to age spots or liver spots that many individuals experience as they grow older. Additionally, skin injuries—such as cuts, burns, or acne—can result in post-inflammatory hyperpigmentation. This occurs when the skin heals and deposit excess melanin at the site of the injury.
Genetic predisposition is also a crucial aspect of hyperpigmentation. Certain individuals may be more likely to experience pigmentation disorders due to their family history. Furthermore, some medications, particularly those that increase sensitivity to sunlight, can exacerbate pigmentation issues. Understanding these causes is essential for effective prevention and treatment of hyperpigmentation.
Risk Factors and Populations at Higher Risk
Hyperpigmentation, characterized by patches of skin that become darker than the surrounding areas, can affect individuals across various demographics. However, certain populations exhibit a higher propensity for developing this skin condition. One of the most prominent risk factors is skin type; individuals with darker skin tones, specifically those with Fitzpatrick skin types IV to VI, are more susceptible to hyperpigmentation. This susceptibility stems from greater melanin production, which, while providing some protection against UV radiation, can lead to excess pigmentation in response to skin injury or inflammation.
Moreover, hormonal fluctuations, particularly in women, serve as another significant risk factor. Conditions such as pregnancy, menopause, and hormonal treatments can trigger melasma, a specific type of hyperpigmentation. Melasma typically appears on the face, often exacerbated by sun exposure, making women in this demographic particularly vulnerable. Additionally, women taking oral contraceptives may also experience instances of hyperpigmentation due to hormonal changes.
Beyond demographic considerations, lifestyle factors play a crucial role in developing hyperpigmentation. A lack of effective sun protection, such as sunscreen or protective clothing, can significantly increase the risk. Ultraviolet (UV) rays stimulate melanin production; therefore, unprotected exposure to the sun can lead to various forms of pigmentation, including age spots and post-inflammatory hyperpigmentation. Furthermore, inadequate skin care routines, which fail to include regular exfoliation and moisturization, can contribute to the buildup of dead skin cells and worsen the appearance of hyperpigmentation. These lifestyle choices highlight the importance of proactive skin care measures in mitigating risk.

Diagnosis of Hyperpigmentation
The diagnosis of hyperpigmentation typically involves a comprehensive evaluation by a dermatologist, who will first conduct a detailed visual examination of the affected skin areas. During this assessment, the clinician will observe the coloration, texture, and distribution of the hyperpigmented lesions. The dermatologist will also take into account the medical history of the patient, including any previous skin conditions, medications, and lifestyle factors that may contribute to the onset of hyperpigmentation.
To differentiate among the various types of hyperpigmentation—such as solar lentigines, post-inflammatory hyperpigmentation, and melasma—the dermatologist may use specific diagnostic tools. A Wood’s lamp examination can be employed to analyze the skin under ultraviolet light, assisting in the identification of deeper pigment changes that may not be visible under standard lighting. Additionally, dermoscopy can be utilized to provide a more detailed view of the skin’s surface and structures, helping to distinguish between hyperpigmentation and other skin disorders like eczema or psoriasis.
In certain cases, a skin biopsy may be necessary to obtain a definitive diagnosis. This procedure involves removing a small sample of the affected skin for laboratory analysis. A skin biopsy can effectively rule out other dermatological conditions, such as melanoma or other types of skin cancer that may present similarly to hyperpigmentation. Once a diagnosis is confirmed, the dermatologist can formulate an appropriate treatment plan tailored to the specific type of hyperpigmentation and the patient’s individual needs, which may include topical treatments, chemical peels, or laser therapies.
Treatment Options for Hyperpigmentation
Hyperpigmentation, a common skin condition characterized by dark patches or spots, can be effectively treated through various methods. The treatments typically fall into two categories: topical treatments and procedural options. Each treatment targets the melanin production that causes the discoloration, and the choice may depend on the severity of the condition and individual skin types.
Topical treatments are often the first line of defense against hyperpigmentation. Hydroquinone is one of the most widely used skin-lightening agents, known for its ability to inhibit melanin production. This treatment is commonly prescribed in concentrations ranging from 2% to 4%. However, prolonged use can lead to side effects, which is why it’s advisable to use it under dermatological guidance. Retinoids, including tretinoin, are another effective topical option. They promote cell turnover and enhance skin texture while minimizing discoloration. Vitamin C, a potent antioxidant, also plays a significant role in diminishing dark spots by inhibiting melanin synthesis and protecting against UV damage.
For those seeking more immediate results, procedural options may be considered. Chemical peels involve the application of a solution that exfoliates the skin’s outermost layers, revealing fresher skin beneath. Various acids, such as glycolic or salicylic acid, are utilized depending on the depth of the peel required. Laser therapy is another advanced treatment option; it uses focused light to break down excess melanin while sparing the surrounding tissue. Research has shown that both chemical peels and laser treatments yield favorable outcomes for hyperpigmentation, providing significant improvement in skin tone.
In summary, the treatments for hyperpigmentation are diverse, making it essential for individuals to consult with a dermatologist to determine the most effective approach tailored to their specific needs and skin conditions. Various options, including topical treatments and procedural interventions, offer promising results with appropriate clinical evidence supporting their efficacy.
Preventive Measures Against Hyperpigmentation
Preventing hyperpigmentation is crucial for maintaining even skin tone and overall skin health. One of the most effective strategies involves diligent sun protection. Ultraviolet (UV) rays from the sun can trigger increased melanin production, leading to dark spots and uneven pigmentation. Therefore, applying a broad-spectrum sunscreen with a minimum SPF of 30 is essential. This helps shield the skin from both UVA and UVB rays, which can contribute significantly to the development of hyperpigmentation.
In addition to sunscreen application, wearing protective clothing can further minimize skin exposure to harmful solar radiation. Wide-brimmed hats, long-sleeved shirts, and sunglasses not only provide additional coverage but also enhance the protective measures of sunscreen. It is advisable to choose clothing made from tightly woven fabrics, which can block more UV rays than loosely woven textiles.
Avoiding peak sun exposure hours is another vital preventive measure. UV rays are typically strongest between 10 a.m. and 4 p.m. By staying indoors or seeking shade during these times, individuals can significantly reduce their risk of hyperpigmentation. Furthermore, those who must be outdoors during these hours should reapply sunscreen every two hours or more frequently if swimming or sweating.
Establishing a proper skincare routine also plays a critical role in preventing hyperpigmentation. Gently cleansing the skin and regularly moisturizing helps to maintain its health and resilience against environmental stressors. Incorporating products that contain antioxidants, vitamins, and exfoliating agents can further enhance skin health and prevent the exacerbation of pigmentation issues. Ultimately, a combination of sun protection strategies and a consistent skincare regimen can serve as effective preventive measures against hyperpigmentation.

Lifestyle Changes for Healthy Skin
Maintaining healthy skin is essential for reducing the risk of hyperpigmentation and enhancing overall skin appearance. One of the foundational aspects is proper hydration. Adequate water intake helps to keep the skin well-hydrated, improving its elasticity and appearance. It is generally recommended to consume at least eight glasses of water daily, though individual needs may vary based on activity levels and environmental factors. Proper hydration ensures that toxins are flushed from the body, contributing to clearer skin and reducing the likelihood of dark spots.
Nutrition also plays a crucial role in maintaining skin health. A balanced diet rich in antioxidants, vitamins, and minerals can significantly influence skin appearance. Foods such as fruits, vegetables, and whole grains provide essential nutrients that support skin repair and regeneration. For instance, vitamin C is known for its ability to brighten the skin and minimize the effects of hyperpigmentation, while vitamin E helps protect against UV damage. Incorporating omega-3 fatty acids from sources like fish and nuts can also support skin barrier function, making the skin less prone to pigmentation issues.
Stress management is another essential aspect of skin health. Chronic stress can lead to hormonal changes that may trigger or worsen hyperpigmentation. Practicing stress-reduction techniques such as yoga, meditation, or deep breathing can help maintain hormonal balance and improve the skin’s overall tone. Additionally, adequate sleep not only aids in stress reduction but also allows for skin regeneration and repair, further promoting a healthy complexion.
Finally, establishing a regular skincare routine is critical. This includes cleansing, exfoliating, and moisturizing, combined with the application of broad-spectrum sunscreen. Adopting such practices can safeguard against sun exposure, which is a primary contributor to hyperpigmentation. By integrating these lifestyle changes, individuals can foster a holistic approach to skin care and create an environment conducive to healthier skin.
Frequently Asked Questions (FAQs)
Hyperpigmentation is a common skin condition that raises numerous questions among those affected. Here, we address some of the most frequently asked questions to provide clarity and guidance.
Is hyperpigmentation permanent?
Hyperpigmentation can be temporary or permanent depending on its cause. Conditions such as sun exposure and inflammation might lead to temporary changes in skin coloration, while post-inflammatory hyperpigmentation may take several months to fade. However, more persistent forms, like melasma, can be more difficult to treat and may require ongoing management. It is advisable to consult a dermatologist for a clearer understanding of individual cases.
Can I use makeup to cover it?
Yes, makeup can be used effectively to cover hyperpigmentation. Many foundation products are formulated with pigments that help mask uneven skin tones. It’s recommended to choose products that are specifically designed for sensitive skin and contain beneficial ingredients such as antioxidants. Additionally, using color-correcting primers can help neutralize darker spots. However, while makeup can provide immediate coverage, it does not address the underlying issues causing hyperpigmentation.
What are the best treatments for hyperpigmentation?
Treatments for hyperpigmentation vary based on its type and severity. Common options include topical creams containing ingredients such as hydroquinone, kojic acid, and retinoids, which work to lighten dark spots. Other effective treatments include chemical peels and laser therapy, which can improve skin tone and texture. Consulting with a healthcare professional is crucial to determine the most suitable treatment plan tailored to individual skin types.
Can hyperpigmentation occur in all skin types?
Yes, hyperpigmentation can affect individuals of all skin types and tones, though its appearance may be more prominent in darker skin. The underlying causes, such as sun exposure, hormones, and inflammatory skin conditions, do not discriminate between skin types. This broad susceptibility underscores the importance of preventive measures and early intervention strategies.
What are the main causes of hyperpigmentation?
Hyperpigmentation occurs when an excess of melanin, the pigment responsible for skin color, is produced. The main causes include sun exposure, which leads to age spots or sun spots, hormonal changes like pregnancy or birth control (which can trigger melasma), and inflammation from skin injuries, acne, or certain skin conditions. Genetics and certain medications can also play a role. Identifying the cause of hyperpigmentation is essential in choosing the right treatment approach.
Can lifestyle changes help reduce hyperpigmentation?
Yes, lifestyle changes can significantly help in managing and reducing hyperpigmentation. Protecting the skin from the sun by using sunscreen daily with SPF 30 or higher can prevent further darkening of spots. Additionally, avoiding smoking, managing stress, staying hydrated, and eating a balanced diet rich in antioxidants can promote healthier skin. Adopting a gentle skincare routine and avoiding picking at skin blemishes can also prevent further pigmentation.
As we delve deeper into understanding hyperpigmentation, it becomes clear that awareness and informed actions can lead to effective management and treatment. By addressing these common questions, we empower individuals with the knowledge necessary to tackle this condition effectively.
When to Consult a Dermatologist
Hyperpigmentation can manifest in various forms, and while it may often be benign, there are specific signs that warrant a consultation with a dermatologist. Recognizing when to seek professional help is essential for both diagnosis and treatment, helping to mitigate any potential underlying skin conditions. One of the key indicators is the presence of rapidly changing pigmentation. If you notice that a mole or pigmented area is changing color, size, or texture, this could be a sign of a more serious skin concern, such as skin cancer. Timely evaluation is crucial as it allows for early intervention, which significantly improves outcomes.
Persistent discoloration that does not respond to over-the-counter treatments is another important reason to contact a skincare professional. It is not uncommon for individuals to experience pigmented areas that fade over time; however, when hyperpigmentation persists despite attempts to treat it with topical agents or skin-care routines, this signals a need for deeper investigation. A dermatologist can offer customized treatment options that might include prescription medications, topical treatments, or even in-office procedures that are more effective than at-home remedies.
Additionally, if hyperpigmentation is accompanied by other symptoms such as itching, pain, or swelling, it’s essential to consult a dermatologist without delay. These symptoms may indicate a dermatological condition that requires immediate attention. Lastly, individuals who have a history of skin cancer or other skin conditions should be proactive in seeking regular evaluations to monitor any changes in pigmentation, enabling a professional to assess these risks promptly and accurately.
Being aware of these indicators can significantly impact your skin health and overall well-being, ensuring that any necessary treatments are started as soon as possible.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

