What is Vestibular Schwannoma?
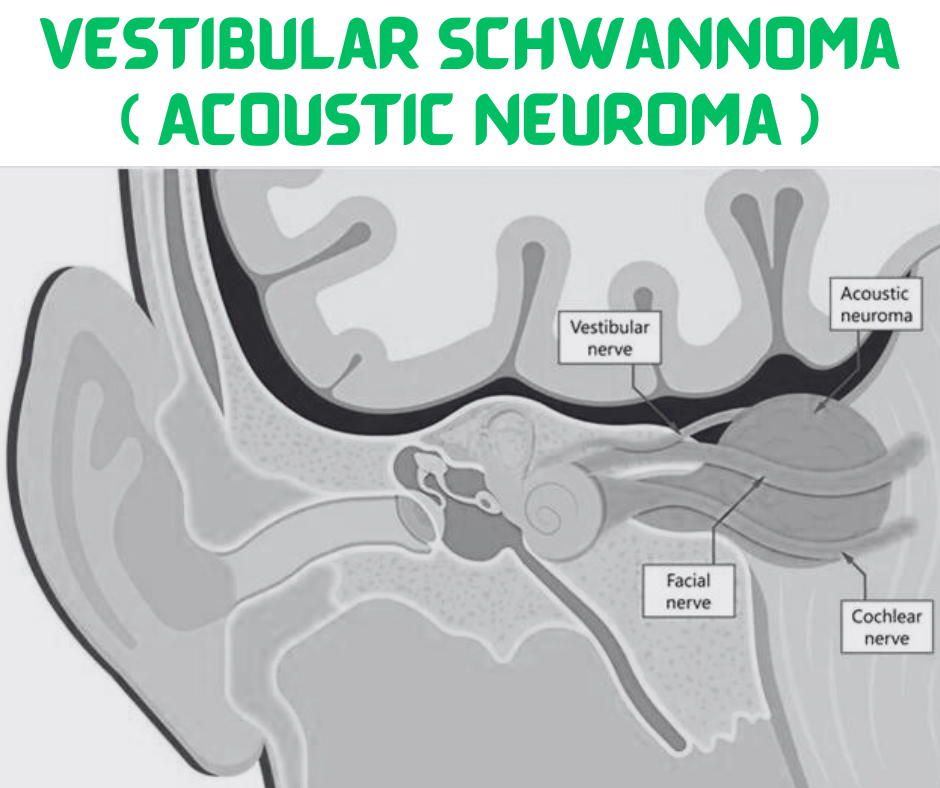
Vestibular schwannoma, commonly referred to as acoustic neuroma, is a benign tumor that arises from Schwann cells, which are critical for the myelination of nerves. This tumor predominantly develops on the vestibulocochlear nerve, also known as cranial nerve VIII, which plays a key role in controlling auditory and balance functions. Although classified as benign, vestibular schwannomas can cause significant health complications due to their location, as they may exert pressure on nearby structures in the brain and ear.
Typically, vestibular schwannomas grow slowly, often remaining asymptomatic for years before symptoms become apparent. As the tumor enlarges, it can affect hearing, balance, and equilibrium. Common initial symptoms include hearing loss, tinnitus (ringing in the ears), and issues with balance. The gradual onset of these symptoms can often lead to delayed diagnosis, as individuals may attribute them to other age-related changes or less critical conditions.
The growth patterns of vestibular schwannomas vary significantly from person to person. While some tumors may remain small and stable, others can grow rapidly, necessitating closer monitoring and, in some cases, intervention. Depending on their size and the degree of impact on auditory and vestibular functions, these tumors may require different approaches to treatment ranging from observation to surgical intervention.
In essence, vestibular schwannoma is a unique type of tumor that, despite its non-cancerous nature, can have profound effects on an individual’s quality of life due to its implications on hearing and balance. Understanding its characteristics is crucial for timely diagnosis and appropriate management of the condition.
Causes and Risk Factors
Vestibular schwannoma, commonly referred to as acoustic neuroma, is a benign tumor that develops on the vestibulocochlear nerve, which is responsible for balance and hearing. While the exact cause of this tumor is not fully understood, specific genetic predispositions and environmental factors have been identified as potential contributors.
One of the most significant genetic risk factors for developing vestibular schwannoma is Neurofibromatosis type II (NF2). This genetic disorder, which is inherited in an autosomal dominant manner, predisposes individuals to develop bilateral vestibular schwannomas, typically starting in young adulthood. NF2 is caused by mutations in the NF2 gene, which is crucial for the regulation of cell growth. Consequently, individuals with this disorder require ongoing monitoring for the development of tumors.
Aside from genetic conditions, there are other potential risk factors that may influence the development of vestibular schwannoma. Some studies suggest that prolonged exposure to certain environmental factors, such as hazardous chemicals or noise pollution, could contribute to the risk, although further research is needed to establish a definitive link. It is important to note that the general population has a low incidence rate of vestibular schwannoma, further illustrating the rarity of this condition.
Additionally, certain demographic factors have also been noted in research. Vestibular schwannomas appear to occur more frequently in adults, particularly in those aged between 30 and 60 years. There is also a slight predominance in females compared to males. Understanding these causes and risk factors is essential for early detection, diagnosis, and potential intervention, as monitoring at-risk individuals can play a crucial role in managing this condition effectively.
Symptoms of Vestibular Schwannoma
Vestibular schwannoma, often referred to as acoustic neuroma, typically manifests through a range of symptoms that can significantly impact an individual’s quality of life. One of the most common symptoms associated with vestibular schwannoma is hearing loss. This hearing impairment usually occurs on one side and may initially present as difficulty hearing in noisy environments or a sensation of fullness in the ear. Over time, this could progress to more pronounced hearing deficits.
Another prevalent symptom is tinnitus, characterized by the perception of ringing, buzzing, or hissing sounds in the ear. This phenomenon can be persistent and may worsen as the tumor grows, contributing to an increase in discomfort and irritation for those affected. Tinnitus can also amplify feelings of anxiety and frustration, which may further detract from daily activities.
Dizziness and balance issues are additional symptoms that individuals with vestibular schwannoma may experience. Dizziness refers to a sense of unsteadiness or vertigo that can lead to difficulty maintaining balance. As the tumor puts pressure on the balance nerve, patients may find it increasingly challenging to walk straight or perform tasks that require coordination. These balance disorders can severely limit an individual’s ability to engage in physical activities and may lead to falls.
The severity of these symptoms can vary significantly among patients, with some experiencing mild disruptions in daily life while others face severe repercussions. Early recognition and assessment of symptoms are crucial, as timely intervention can lead to improved outcomes. Understanding these symptoms is vital for patients and healthcare providers alike, ensuring appropriate actions can be taken for management and treatment of vestibular schwannoma.

Diagnosis of Vestibular Schwannoma
The diagnostic process for vestibular schwannoma begins with a thorough medical history assessment. During this initial evaluation, healthcare professionals inquire about the patient’s symptoms, focusing on hearing loss, tinnitus, balance difficulties, and any associated neurological symptoms. The elicitation of a detailed symptom history aids in establishing a clinical suspicion of vestibular schwannoma.
Subsequently, a comprehensive physical examination is performed. This examination commonly includes neurological assessments to evaluate the patient’s cranial nerve function, particularly those associated with hearing and balance, such as the auditory and vestibular nerves. Any noticeable abnormalities during the examination may further warrant advanced imaging studies to determine the presence of a vestibular schwannoma.
To confirm the diagnosis and provide critical information regarding tumor size and location, imaging techniques are essential. Magnetic Resonance Imaging (MRI) is the gold standard for visualizing vestibular schwannomas, offering high-resolution images that aid in distinguishing tumors from adjacent structures. MRI scans can effectively reveal the characteristic features of vestibular schwannomas and are particularly useful for monitoring tumor growth over time. In certain cases, when MRI is contraindicated, Computed Tomography (CT) scans may be utilized as an alternative, though they offer less detailed visualization compared to MRI.
Enhancing the diagnostic accuracy may involve using contrast agents during the imaging procedures, which enhances the visibility of tumors and enables better characterization. The combination of detailed medical history, systematic physical examination, and advanced imaging techniques provides a comprehensive approach to diagnosing vestibular schwannoma, ultimately leading to timely intervention.
Treatment Options for Vestibular Schwannoma
Vestibular schwannoma (VS), also known as acoustic neuroma, presents various treatment options dependent on the tumor’s size, location, and the patient’s overall health and preferences. The primary strategies include observation, surgical removal, and radiation therapy.
Observation is often recommended for patients with small vestibular schwannomas, particularly if symptoms are minimal or non-existent. This management approach involves regular monitoring through MRI scans and hearing tests. The advantage of this method lies in its non-invasive nature; however, it carries the risk of tumor growth, which may eventually necessitate intervention if symptoms develop or worsen.
For patients experiencing significant symptoms or for larger vestibular schwannomas, surgical removal is a viable option. Neurosurgeons may perform a craniotomy or use a less invasive technique called keyhole surgery, depending on the tumor’s characteristics. The main advantage of surgical removal is the potential for complete excision of the tumor, which may alleviate or prevent further neurological deficits. However, surgery is associated with risks such as hearing loss, facial nerve injury, or balance problems, which can significantly impact the patient’s quality of life.
Radiation therapy, particularly stereotactic radiosurgery (SRS), is another treatment modality for vestibular schwannomas. This non-invasive technique delivers high doses of radiation precisely targeting the tumor while sparing surrounding healthy tissue. The primary advantage of SRS is its ability to halt tumor growth with a relatively low complication rate. However, it may not entirely remove the tumor and could potentially lead to delayed side effects, such as radiation-induced changes in hearing or balance.
Ultimately, treatment options for vestibular schwannoma vary based on individual circumstances, and a comprehensive discussion with an otolaryngologist and neurosurgeon is essential to choose the most appropriate approach.
Possible Complications and Prognosis
Vestibular schwannoma, also known as acoustic neuroma, is a benign tumor that develops on the vestibulocochlear nerve, which is responsible for hearing and balance. While these tumors are non-cancerous, they can lead to several complications that significantly impact an individual’s quality of life. One of the most common complications associated with vestibular schwannoma is hearing loss. This can occur due to the tumor pressing against the cochlear branch of the vestibulocochlear nerve, leading to progressive or sudden deafness in the affected ear. In some cases, hearing aids may be necessary to manage the resultant auditory challenges.
Another potential complication is facial nerve damage, which can manifest as facial weakness or paralysis, affecting the ability to make facial expressions and perform basic functions such as closing the eyes. This occurs when the tumor compresses the facial nerve, leading to varying degrees of dysfunction. Furthermore, balance problems are prevalent, as the vestibular component of the vestibulocochlear nerve can be impacted. Individuals may experience vertigo, dizziness, or unsteadiness, which can significantly hinder daily activities.
The prognosis for individuals diagnosed with vestibular schwannoma varies depending on several factors. The size and location of the tumor, the age of the patient, and overall health can all influence outcomes. Smaller tumors, especially when detected early, tend to have better prognoses, allowing for effective treatment options that can preserve hearing and minimize complications. Conversely, larger tumors may require more aggressive interventions, such as surgery or radiation therapy, potentially resulting in a higher risk of complications. Continuous monitoring and follow-up care are crucial to ensure optimal outcomes and identify any complications early in the patient’s treatment path.

Coping Strategies for Living with Vestibular Schwannoma
Living with vestibular schwannoma can be challenging due to the various symptoms it presents, including hearing loss, tinnitus, and balance issues. However, implementing effective coping strategies can significantly improve one’s quality of life. One of the first steps is to embrace lifestyle adjustments tailored to your individual needs. Regular check-ups with healthcare providers allow for the monitoring of symptoms, allowing patients to manage them proactively. Establishing a routine that includes physical activity can help enhance balance and strengthen surrounding muscles, ultimately reducing fall risk.
Additionally, dietary considerations may play a role in overall health management. Maintaining a balanced diet rich in vitamins and minerals can boost energy levels and contribute to a sense of well-being. Staying hydrated and limiting caffeine and alcohol can also help mitigate some symptoms, such as dizziness and tinnitus. Mindfulness practices, such as yoga and meditation, can greatly assist in managing stress, which is essential as anxiety can exacerbate symptoms associated with vestibular schwannoma.
Another invaluable coping strategy involves creating a strong support network. Connecting with friends, family, or support groups allows individuals to share their experiences and receive emotional support. Online forums and local support groups specifically focused on vestibular disorders can provide encouragement and advice. Therapy or counseling services can also be beneficial, offering a safe space for individuals to express their feelings and develop coping techniques.
Lastly, exploring therapeutic options such as vestibular rehabilitation therapy (VRT) can offer significant advantages. VRT practices help improve balance and reduce dizziness through tailored exercises. In conclusion, by implementing these coping strategies, individuals diagnosed with vestibular schwannoma can enhance their quality of life, managing their symptoms more effectively while fostering a comprehensive support system.
Current Research and Future Directions
Recent advancements in the field of vestibular schwannoma (VS) research have opened new avenues for understanding this complex condition and improving treatment outcomes. Ongoing clinical trials are focusing on various aspects, including novel therapeutic agents, monitoring techniques, and long-term management strategies. Researchers are particularly interested in the molecular biology of vestibular schwannomas, aiming to identify potential biomarkers that could help in predicting tumor behavior and patient prognosis.
One area of current research involves targeted therapies that aim to inhibit specific pathways associated with the growth of vestibular schwannomas. For instance, the use of agents that target the tumor’s genetic mutations, such as the NF2 gene, is being explored. These targeted approaches could offer more personalized treatment options, addressing the underlying causes of tumor progression rather than only managing symptoms. Moreover, several studies are investigating the efficacy of stereotactic radiosurgery and its role in preserving hearing while controlling tumor growth, leading to improved quality of life for patients.
Additionally, the integration of advanced imaging techniques is enhancing our understanding of vestibular schwannoma. For example, researchers are employing diffusion-weighted imaging and volumetric analysis to analyze tumor dynamics more precisely. This can assist in making timely decisions regarding intervention, which is crucial for optimal patient outcomes. Furthermore, interdisciplinary collaborations involving otolaryngologists, neuro-oncologists, and radiologists are facilitating a holistic approach to treatment and research.
Looking towards the future, there is a clear need for continued innovation in the management of vestibular schwannoma. The ongoing exploration of both surgical techniques and non-invasive treatment options signifies a promising horizon for patients. As clinical trials yield more data, healthcare providers can aim for tailored treatment plans that cater to individual patient needs, ultimately improving the overall prognosis and life quality of those affected by vestibular schwannoma.
Frequently Asked Questions (FAQs)
Vestibular schwannoma, commonly referred to as acoustic neuroma, is a benign tumor that develops on the vestibulocochlear nerve, which is responsible for balance and hearing. This section addresses prevalent inquiries regarding the diagnosis, associated risks, and management of vestibular schwannoma.
How is vestibular schwannoma diagnosed?
Diagnosis typically begins with a thorough medical history and a physical examination. If a medical professional suspects vestibular schwannoma, imaging tests such as MRI or CT scans are often utilized. These scans provide detailed images of the brain and can reveal the presence of tumors, helping clinicians make an accurate diagnosis. Diagnostic audiometry may also be performed to assess hearing ability and identify potential function loss related to the tumor’s pressure on the cochlear nerve.
What are the potential risks associated with vestibular schwannoma?
While vestibular schwannomas are benign, they can grow and exert pressure on nearby structures, leading to complications. Potential risks include hearing loss, tinnitus (ringing in the ears), balance issues, and, in some cases, facial nerve dysfunction if the tumor grows large enough. Regular monitoring and appropriate management are crucial to minimize these risks.
What management strategies are available for vestibular schwannoma?
Management strategies for vestibular schwannoma depend on factors such as tumor size, growth rate, and the patient’s overall health. Options include active surveillance, surgical removal, and radiation therapy. Active surveillance involves regular monitoring of the tumor with periodic imaging, particularly for smaller tumors that are not causing significant symptoms. Surgical options may be considered for larger tumors, aiming to preserve hearing and facial nerve function. Radiation therapy, such as stereotactic radiosurgery, may also be an effective treatment for patients seeking a non-invasive approach.
Can vestibular schwannoma be prevented?
There are no known preventive measures for vestibular schwannoma, as its exact cause is not fully understood. However, individuals with a family history of neurofibromatosis type 2 (NF2), a genetic disorder associated with bilateral vestibular schwannomas, may benefit from genetic counseling. Early detection through routine hearing assessments and medical checkups can help identify the condition before symptoms become severe.
What are the long-term effects of vestibular schwannoma treatment?
The long-term effects depend on the chosen treatment approach. Patients undergoing active surveillance may experience gradual hearing loss or balance issues if the tumor grows. Surgical removal carries potential risks such as facial nerve weakness, hearing impairment, or cerebrospinal fluid leakage. Radiation therapy may stabilize tumor growth but can also lead to delayed nerve damage. Post-treatment rehabilitation, including physical therapy and hearing aids, may help manage lingering symptoms and improve quality of life.
Addressing concerns through these frequently asked questions can help individuals better understand vestibular schwannoma and the associated management options.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

