Decoding Vestibular Schwannoma: A Comprehensive Exploration
In the realm of neurological disorders, Vestibular Schwannoma, commonly known as Acoustic Neuroma, stands as a unique and intriguing challenge. Nestled within the intricate folds of the human ear, this benign tumor has the potential to disrupt not only one’s auditory experience but also various facets of daily life. In this blog post, we will delve into the nuances of Vestibular Schwannoma, exploring its origins, symptoms, diagnosis, and treatment options.
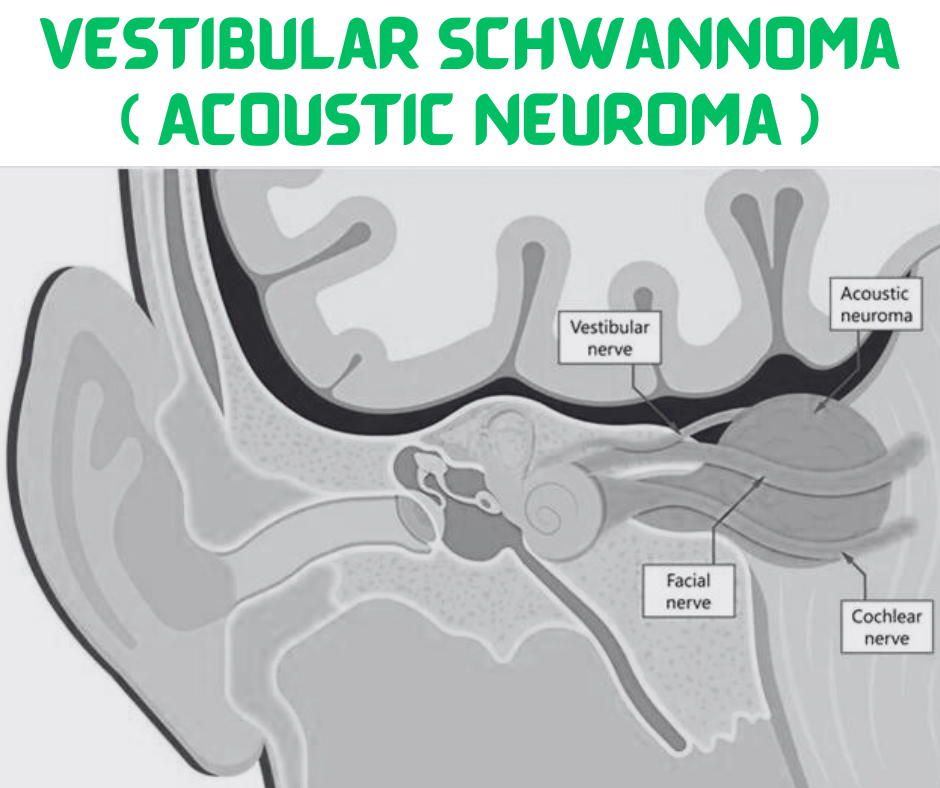
Understanding Vestibular Schwannoma
Vestibular Schwannoma is a noncancerous, slow-growing tumor that develops on the vestibular nerve, responsible for transmitting balance and spatial information from the inner ear to the brain. Despite its benign nature, the tumor’s location within the narrow confines of the internal auditory canal can lead to compression of adjacent structures, primarily the eighth cranial nerve responsible for hearing.
Symptoms
Here are some common symptoms associated with Vestibular Schwannoma:
- Gradual Hearing Loss:
- One of the hallmark symptoms is a slow and progressive loss of hearing, typically affecting one ear. The hearing loss often begins with high-pitched sounds and may eventually lead to total deafness in the affected ear.
- Tinnitus:
- Many individuals with Vestibular Schwannoma experience tinnitus, a persistent ringing, buzzing, or hissing sound in the affected ear. Tinnitus can be constant or intermittent and may be more noticeable in quiet environments.
- Balance Issues:
- The tumor’s location on the vestibular nerve can lead to imbalance and coordination problems. Individuals may experience a feeling of unsteadiness, especially during sudden head movements. Vertigo, a sensation of spinning or dizziness, can also occur.
- Facial Weakness or Numbness:
- Larger tumors may exert pressure on the facial nerve, resulting in facial weakness or numbness on one side of the face. This can affect expressions and facial muscle control.
- Headaches:
- Some individuals with Vestibular Schwannoma may experience headaches, particularly if the tumor causes increased pressure within the skull.
- Ear Fullness or Pressure:
- Patients may report a sensation of fullness or pressure in the affected ear, even if there is no visible blockage. This can contribute to discomfort and may be accompanied by a feeling of congestion.
- Changes in Vision or Difficulty Swallowing:
- In rare cases, larger tumors may compress adjacent nerves, leading to changes in vision or difficulty swallowing.
It’s important to note that Vestibular Schwannoma symptoms typically develop slowly, and some individuals may not experience noticeable symptoms until the tumor reaches a significant size. Additionally, not all individuals with Vestibular Schwannoma will exhibit the same set of symptoms.
Diagnosis
The diagnosis of Vestibular Schwannoma (Acoustic Neuroma) involves a combination of clinical evaluation, audiometric tests, and imaging studies. Here’s an overview of the diagnostic process:
1. Clinical Evaluation:
- Medical History: The physician will inquire about the patient’s medical history, paying close attention to symptoms such as hearing loss, tinnitus, balance issues, and facial weakness.
- Physical Examination: A thorough neurological examination may be conducted to assess facial nerve function, balance, and coordination.
2. Audiometric Tests:
- Pure-Tone Audiometry: This test measures the ability to hear different tones and pitches. Individuals with Vestibular Schwannoma often exhibit a specific pattern of hearing loss, typically affecting higher frequencies initially.
- Speech Audiometry: Assessing the ability to hear and understand speech is an integral part of the audiometric evaluation.
- Auditory Brainstem Response (ABR) Test: This specialized test measures the electrical activity of the auditory nerve and brainstem in response to sound. It can help evaluate the integrity of the auditory pathway.
3. Imaging Studies:
- Magnetic Resonance Imaging (MRI): This is the primary imaging modality used to visualize Vestibular Schwannomas. A contrast-enhanced MRI provides detailed images of the internal auditory canal and surrounding structures, helping to determine the size, location, and impact of the tumor. The use of contrast allows for better visualization of the tumor against surrounding tissues.
4. Electronystagmography (ENG) or Videonystagmography (VNG):
- These tests evaluate eye movements to assess vestibular function. Abnormal eye movements may indicate issues with the vestibular nerve, providing additional information for diagnosis.
5. Computed Tomography (CT) Scan:
- While MRI is the preferred imaging modality, a CT scan may be used in certain cases to provide additional information about bone structures and rule out other conditions.
6. Evoked Potentials:
- Tests such as the somatosensory evoked potential (SSEP) or visual evoked potential (VEP) may be employed to assess the function of nerves related to touch or vision.
7. Laboratory Tests:
- Blood tests are generally not used to diagnose Vestibular Schwannoma, but they may be conducted to rule out other medical conditions.
8. Monitoring and Follow-up:
- In cases where the tumor is small and not causing significant symptoms, a “watch and wait” approach may be adopted. Regular monitoring through imaging studies, usually MRI, helps track the tumor’s growth.
Treatment Options
The management of Vestibular Schwannoma (Acoustic Neuroma) depends on several factors, including the size of the tumor, the patient’s overall health, and the presence and severity of symptoms. Treatment options can vary, and the decision is often made collaboratively between the patient and a multidisciplinary healthcare team. Here are the primary treatment options for Vestibular Schwannoma:
1. Observation (Watchful Waiting):
- Indications: Small tumors or tumors with minimal or no symptoms.
- Rationale: Monitoring the tumor’s growth through regular imaging studies (typically MRI) without immediate intervention. This approach is suitable for patients with slow-growing tumors who may not experience significant symptoms.
2. Surgery:
- Indications: Larger tumors, tumors causing significant symptoms, or tumors in patients who prefer a definitive intervention.
- Types of Surgery:
- Microsurgery (Translabyrinthine or Suboccipital): Involves the removal of the tumor through a small incision behind the ear or through the skull.
- Middle Fossa Approach: Used for smaller tumors located near the internal auditory canal, with an emphasis on preserving hearing.
- Retrosigmoid Approach: Aims to remove the tumor while preserving facial nerve function.
3. Radiation Therapy:
- Indications: Small to medium-sized tumors, tumors in patients who are not surgical candidates, or in cases where preservation of hearing is a priority.
- Types of Radiation Therapy:
- Stereotactic Radiosurgery (Gamma Knife, CyberKnife): Precisely delivers high doses of radiation to the tumor while minimizing exposure to surrounding tissues.
- Fractionated Stereotactic Radiotherapy: Administers radiation in smaller, divided doses over multiple sessions.
4. Combination Therapies:
- In some cases, a combination of treatments may be recommended, such as surgery followed by radiation therapy.
5. Rehabilitation and Supportive Care:
- Regardless of the chosen treatment, rehabilitation services may be beneficial, especially for individuals who experience balance issues, facial weakness, or hearing loss. Speech therapy, physical therapy, and hearing aids can contribute to improved quality of life.
6. Clinical Trials:
- Participation in clinical trials may be an option for some patients, especially those with recurrent or challenging cases. Clinical trials explore new treatment approaches and medications.
Considerations for Treatment Decision-Making:
- Tumor Size and Growth Rate: The size and growth rate of the tumor play a significant role in determining the appropriate course of action.
- Hearing Preservation: For some patients, especially those with smaller tumors, preserving hearing function may be a crucial consideration in treatment planning.
- Patient Preference: The patient’s preference and overall health are vital factors. Some individuals may prioritize treatments that offer the best chance of preserving quality of life.
- Multidisciplinary Approach: Treatment decisions are often made collaboratively by a team of specialists, including otolaryngologists, neurosurgeons, radiation oncologists, and audiologists.
Vestibular Schwannoma management is highly individualized, and the chosen treatment should align with the patient’s unique circumstances and preferences. Regular follow-up appointments and imaging studies are essential to monitor the tumor’s response to treatment and assess for any recurrence or new developments.
Disclaimer
This blog post is intended for informational purposes only and should not be considered as medical advice. It is crucial to consult with a qualified healthcare professional for accurate diagnosis and appropriate treatment recommendations based on individual circumstances. The information provided here is based on general knowledge and understanding as of the date of writing, and medical practices may evolve over time.
Stay updated—subscribe now for informed empowerment!

