Vestibular System: 7 Shocking Facts You Must Know
Understanding the Vestibular System
The vestibular system is a critical component of the human body, tasked with maintaining balance and spatial orientation. Located within the inner ear, it comprises complex structures such as the semicircular canals, the utricle, and the saccule, which work in tandem to provide essential sensory information. This system enables humans to stabilize their gaze, posture, and movement by detecting changes in head position and motion.
Historically, our understanding of the vestibular system has evolved significantly. The initial discovery dates back to the early 19th century when pioneering scientists like Jean Pierre Flourens began to investigate the intricate relationship between the ear and balance. His groundbreaking experiments on pigeons marked the beginning of a quest to unravel the mysteries of the vestibular apparatus.
Key scientific milestones have punctuated the study of the vestibular system. In the late 19th century, Josef Breuer and Ernst Mach notably contributed by identifying that the semicircular canals sense angular acceleration. Their work laid the foundation for modern vestibular research. Further advancements occurred in the mid-20th century with the introduction of electrophysiological techniques, allowing for a detailed understanding of the neural pathways involved.
Today, the importance of the vestibular system in daily life is widely recognized. It plays a pivotal role not only in balance but also in spatial orientation, allowing humans to navigate their environment with remarkable precision. With ongoing research, the intricate workings of the vestibular system continue to be explored, offering promising potential for innovative treatments and interventions for balance disorders.
Anatomy of the Vestibular System
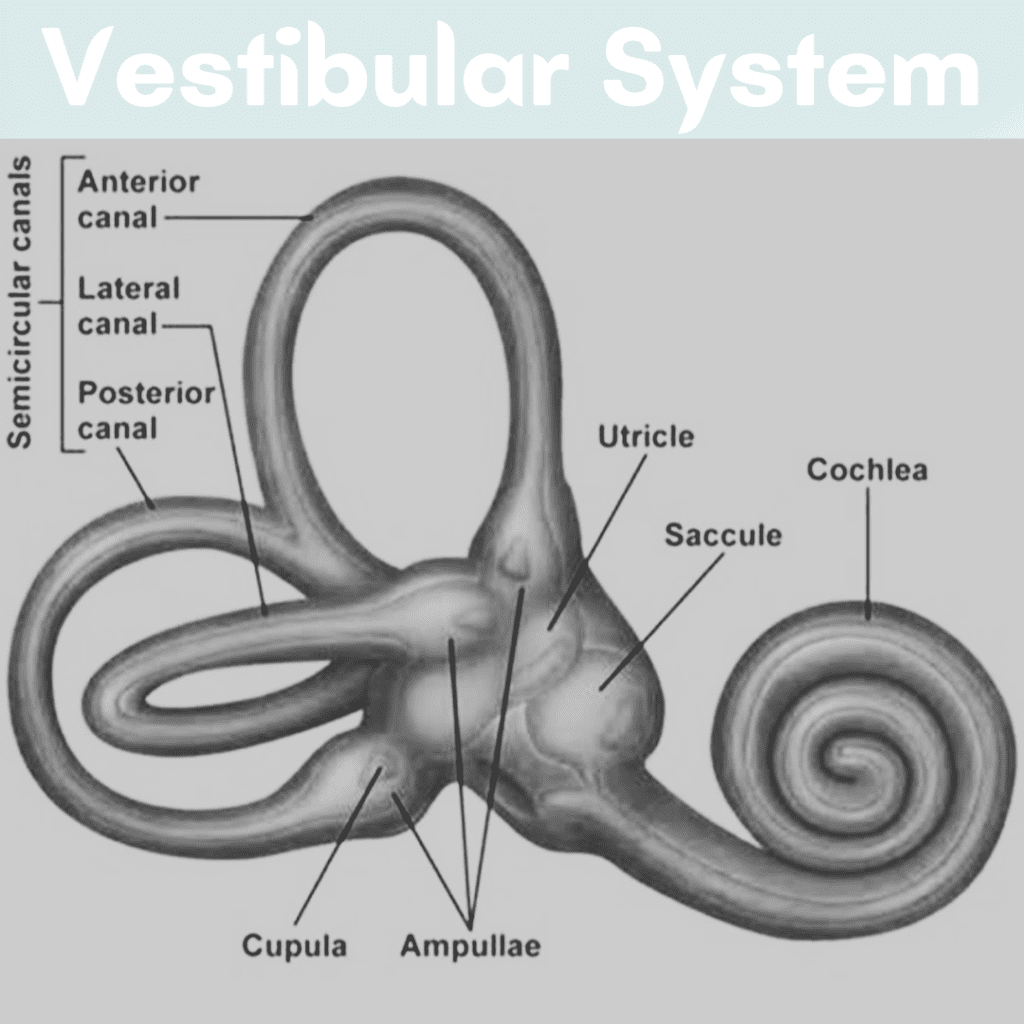
The vestibular system, an intricate component of the inner ear, plays a vital role in maintaining balance and spatial orientation. It comprises several essential structures: the semicircular canals, the otolith organs (utricle and saccule), and their complex connections to the cochlea and brain. Each part works in harmony to detect motion and position, relaying critical information to support equilibrium and coordinated movements.
The semicircular canals are three fluid-filled loops oriented perpendicularly to one another. These canals are crucial for detecting rotational movements or angular acceleration of the head. Inside, tiny hair cells with cilia are embedded in a gelatinous structure called the cupula. As the head rotates, the fluid (endolymph) within the canals shifts, causing the cupula to move and bend the hair cells. This mechanical deformation gets translated into electrical signals, which are then transmitted to the brain via the vestibular nerve.
Adjacent to the semicircular canals are the otolith organs: the utricle and saccule. Unlike the canals, these organs are responsible for detecting linear acceleration and the effects of gravity. Each otolith organ contains a macula, a sensory epithelium covered by otoconia – tiny calcium carbonate crystals. When the head tilts or undergoes linear motion, these crystals shift relative to the gelatinous layer beneath them, distorting the hair cells and initiating neural signals to the brain.
Interconnected with the vestibular structures is the cochlea, primarily responsible for hearing. However, the close proximity and shared fluid systems between the cochlea and the vestibular apparatus facilitate the integration of auditory and vestibular information. This connection underscores the collaborative role of the vestibular system in sensory processing.
Overall, the vestibular system’s anatomical complexity underscores its critical function in maintaining balance and spatial orientation. Its seamless interaction with the brain ensures that our bodies can effectively navigate and respond to dynamic environments.
How the Vestibular System Works
The vestibular system is integral to maintaining balance and spatial orientation, functioning through a complex array of physiological mechanisms. This system is primarily housed within the inner ear, where specialized sensory receptors detect shifts in head motion and orientation. The key structures involved include the semicircular canals, the otolithic organs (utricle and saccule), and the vestibular nerve.
Central to the vestibular system’s operation, the semicircular canals are three looped structures positioned perpendicularly to each other. These canals contain fluid called endolymph. As the head moves, the fluid within these canals shifts, creating a force that displaces tiny hair cells known as cilia located on the crista ampullaris. When these cilia bend, they generate nerve impulses that are then transmitted to the brain via the vestibular nerve, signaling rotational movements.
The otolithic organs, namely the utricle and saccule, are responsible for detecting linear acceleration and head position relative to gravity. Contained within these organs is a gelatinous matrix embedded with calcium carbonate crystals known as otoconia. When the head tilts or experiences linear acceleration, these otoconia shift, causing the cilia within the matrix to bend. This bending converts mechanical energy into electrical signals, which are then sent to the brain to assess dynamic and static equilibrium.
Another critical aspect of the vestibular system is the vestibulo-ocular reflex (VOR). The VOR ensures visual stability by adjusting eye movement in reaction to head motion. For instance, when the head turns to the right, the VOR prompts the eyes to move to the left, thereby maintaining a steady gaze. This reflex is vital for activities that require constant head movement, such as reading or driving, as it allows for a stable visual field.
In essence, the vestibular system’s intricate network of sensory receptors, fluid-filled canals, and neural connections facilitate our understanding of motion, balance, and spatial orientation, seamlessly integrating these signals to ensure coordinated movement and equilibrium.

Common Disorders of the Vestibular System
The vestibular system, located in the inner ear, plays a fundamental role in maintaining balance and spatial orientation. Various disorders can affect this intricate system, leading to significant disruptions in an individual’s daily life. Among the most prevalent vestibular disorders are vertigo, Ménière’s disease, vestibular neuritis, and benign paroxysmal positional vertigo (BPPV). Understanding these conditions, their symptoms, and potential causes can provide valuable insights into the challenges faced by those affected.
Vertigo: Vertigo is characterized by an illusion of movement, often described as spinning or swaying, despite a person being stationary. This sensation can be severely disorienting and is commonly caused by issues within the inner ear. Symptoms of vertigo can include dizziness, nausea, vomiting, and difficulty in balancing. Everyday activities such as walking or driving can become hazardous, drastically reducing an individual’s quality of life.
Ménière’s Disease: Ménière’s disease is a chronic condition that affects the inner ear, leading to episodes of vertigo, tinnitus (ringing in the ear), hearing loss, and a feeling of fullness in the affected ear. The exact cause remains unknown, but it is believed to be associated with abnormalities in the fluid dynamics within the inner ear. The unpredictable nature of Ménière’s disease can cause significant stress and anxiety, impacting both personal and professional life.
Vestibular Neuritis: This disorder results from inflammation of the vestibular nerve, which sends balance and head position information from the inner ear to the brain. Often linked to viral infections, vestibular neuritis causes sudden, severe vertigo, dizziness, and balance difficulties. While hearing usually remains unaffected, the intense symptoms may persist for several days, followed by a gradual recovery period. During this time, individuals may find it challenging to perform routine tasks without assistance.
Benign Paroxysmal Positional Vertigo (BPPV): BPPV is one of the most common causes of vertigo, arising from dislodged calcium crystals within the inner ear canals. These misplaced crystals interfere with normal fluid movement, sending false signals to the brain about head position. BPPV episodes are typically brief but triggered by specific head movements, such as looking up or rolling over in bed. Although not life-threatening, BPPV can significantly disrupt daily activities and quality of sleep.
These vestibular disorders underscore the importance of proper diagnosis and management to alleviate symptoms and improve patient outcomes. Enhanced awareness can lead to better support systems and resources for those affected, ultimately fostering a more balanced and fulfilling life.
Diagnostic Methods for Vestibular Disorders
The accurate diagnosis of vestibular disorders involves a combination of clinical evaluations and advanced diagnostic tools. Initially, a detailed medical history and physical examination are conducted to gather symptoms and assess the severity of the condition. This foundational step often guides the choice of specialized diagnostic tests that may follow.
Among the key diagnostic tools, Electronystagmography (ENG) and Videonystagmography (VNG) are commonly employed. ENG measures involuntary eye movements using electrodes placed around the eyes, while VNG employs infrared cameras to meticulously capture and analyze eye movement patterns. Both methods are crucial in detecting abnormal eye movements that may indicate underlying vestibular dysfunction.
Imaging techniques such as Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans play a vital role in the diagnosis process. MRI provides detailed images of the brain and inner ear, allowing for the detection of tumors, inflammatory conditions, or vascular irregularities that could be affecting the vestibular system. CT scans, on the other hand, excel in identifying structural abnormalities and bone-related issues within the inner ear.
Another specialized test is the rotary chair testing, which assesses the vestibulo-ocular reflex by monitoring eye movements while the patient is rotated in a motorized chair. This test is particularly useful in diagnosing bilateral vestibular loss and evaluating the functional status of the entire vestibular system.
Additionally, the head impulse test (HIT) is employed to evaluate the function of the semicircular canals, as it involves quick, passive head movements while observing the patient’s ability to maintain focus on a target. Video head impulse testing (vHIT) is a recent advancement that uses high-speed video technology to provide more precise measurements.
Through these comprehensive diagnostic methods, healthcare professionals are equipped to accurately identify and treat various vestibular disorders, ensuring optimal care and targeted management strategies for affected individuals.
Treatment and Management of Vestibular Disorders
Vestibular disorders, while often distressing, can be managed effectively through a variety of treatment options tailored to the individual needs of patients. The medical treatments for these conditions include medications that can alleviate symptoms such as dizziness and nausea. Commonly prescribed drugs include vestibular suppressants like antihistamines and benzodiazepines, as well as antiemetics for controlling nausea.
Physical therapy, specifically vestibular rehabilitation therapy (VRT), plays a crucial role in the management of vestibular disorders. VRT is a specialized form of therapy designed to improve balance and reduce dizziness-related problems. It involves exercises that aim to desensitize the vestibular system to movements that typically provoke symptoms. Patients often work with physical therapists to perform these exercises, which can significantly enhance their quality of life.
In certain cases where symptoms are severe or persistent, surgical options might be considered. Surgical interventions, such as labyrinthectomy or vestibular nerve section, are generally reserved for patients who do not respond to other treatments. These procedures aim to either partially or entirely disable the defective part of the vestibular system, thereby reducing symptoms.
In addition to medical and surgical treatments, lifestyle changes and coping strategies are essential for long-term management of vestibular disorders. These can include dietary adjustments, like reducing caffeine and alcohol intake, to minimize symptom triggers. Stress management techniques, such as mindfulness and yoga, are also beneficial in mitigating symptoms. Moreover, patients are encouraged to create a safe home environment, free of tripping hazards, to prevent falls and injuries.
Effective management of vestibular disorders often requires a multi-faceted approach combining medication, physical therapy, and sometimes surgery, along with practical lifestyle adjustments to ensure a comprehensive treatment plan. Patients are advised to work closely with healthcare professionals to tailor these strategies to their specific needs for optimal outcomes.

Research and Advances in Vestibular Science
The field of vestibular science has seen significant advancements in recent years, driven by ongoing research and the development of innovative technologies. These advancements contribute to a deeper understanding of the vestibular system and enhance diagnostic and therapeutic options for vestibular disorders, which affect millions globally.
One notable area of progress is the emergence of novel diagnostic tools. Traditional diagnostics often relied on subjective measures and rudimentary tests. However, advancements in imaging technologies, such as functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI), have revolutionized how we assess vestibular function. These tools offer detailed insights into the neural pathways and brain regions involved in vestibular processing, enhancing the accuracy of diagnoses.
In addition to improved diagnostics, new therapies are emerging as a result of cutting-edge research. Vestibular rehabilitation therapy (VRT) remains a cornerstone of treatment; however, advancements in this field have led to more personalized and effective rehabilitation protocols. Virtual reality (VR) therapy, for example, leverages immersive environments to simulate complex motion and spatial orientation scenarios, allowing patients to gradually adapt to vestibular stimuli in a controlled manner. This innovative approach has shown promising results in clinical trials.
Moreover, ongoing studies are investigating the potential of pharmacological interventions targeted at vestibular disorders. Researchers are exploring various medication regimens that aim to alleviate the symptoms of vertigo and balance disorders by modulating neurotransmitter activity within the vestibular system. These efforts are still in the experimental phase, yet they hold the promise of providing new avenues for treatment.
Finally, emerging therapies such as the use of vestibular implants are gaining traction. Similar to cochlear implants used in auditory disorders, vestibular implants are designed to stimulate the vestibular nerve directly, offering a potential new solution for patients with severe, treatment-resistant vestibular dysfunction. Early studies indicate that these implants could significantly improve balance and stability in affected individuals.
Overall, the continuous research and technological advancements in vestibular science are paving the way for a better understanding and management of vestibular disorders. Enhanced diagnostics, innovative therapies, and ongoing clinical studies contribute to a more comprehensive approach, offering renewed hope for patients suffering from these challenging conditions.
FAQ about the Vestibular System
What are some common signs of vestibular dysfunction?
Vestibular dysfunction can manifest through various symptoms, including but not limited to dizziness, vertigo, imbalance, spatial disorientation, and issues with visual stability. Additionally, individuals may experience nausea, vomiting, and difficulties with concentration or memory due to vestibular issues.
How do dizziness and vertigo differ?
Dizziness is a more general term describing feelings of lightheadedness, faintness, or unsteadiness. Vertigo, a subtype of dizziness, refers specifically to the sensation that you, or your environment, is moving or spinning, even when there is no actual movement. Vertigo is often associated with vestibular disorders.
Can vestibular disorders impact the quality of life?
Yes, vestibular disorders can significantly affect quality of life. Chronic dizziness or imbalance can hinder daily activities, work productivity, and social interactions. It may also lead to anxiety, depression, and altered self-perception due to persistent physical and emotional stress.
When should one seek medical advice for vestibular issues?
It is crucial to seek medical advice if you experience persistent dizziness, vertigo, imbalance, or any other symptoms related to vestibular dysfunction. Early diagnosis and treatment can prevent further complications and improve overall quality of life. Immediate medical attention is warranted if these symptoms are accompanied by severe headache, chest pain, or neurological signs like difficulty speaking or weakness.
How are vestibular disorders diagnosed?
Diagnosis typically involves a combination of patient history, physical examination, and specialized tests. These may include vestibular function tests such as electronystagmography (ENG), videonystagmography (VNG), or rotational chair testing. Additionally, imaging techniques like MRI or CT scans may be used to rule out other potential causes.
What are some common treatments for vestibular disorders?
Treatment varies based on the specific condition but can include vestibular rehabilitation therapy (VRT), medications to manage symptoms, and lifestyle adjustments to avoid triggers. In some cases, surgical intervention may be necessary. Audiologists, physical therapists, and specialized healthcare professionals play key roles in developing individualized treatment plans.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

