7 Critical Congenital Conditions You Must Know
Understanding Congenital Conditions
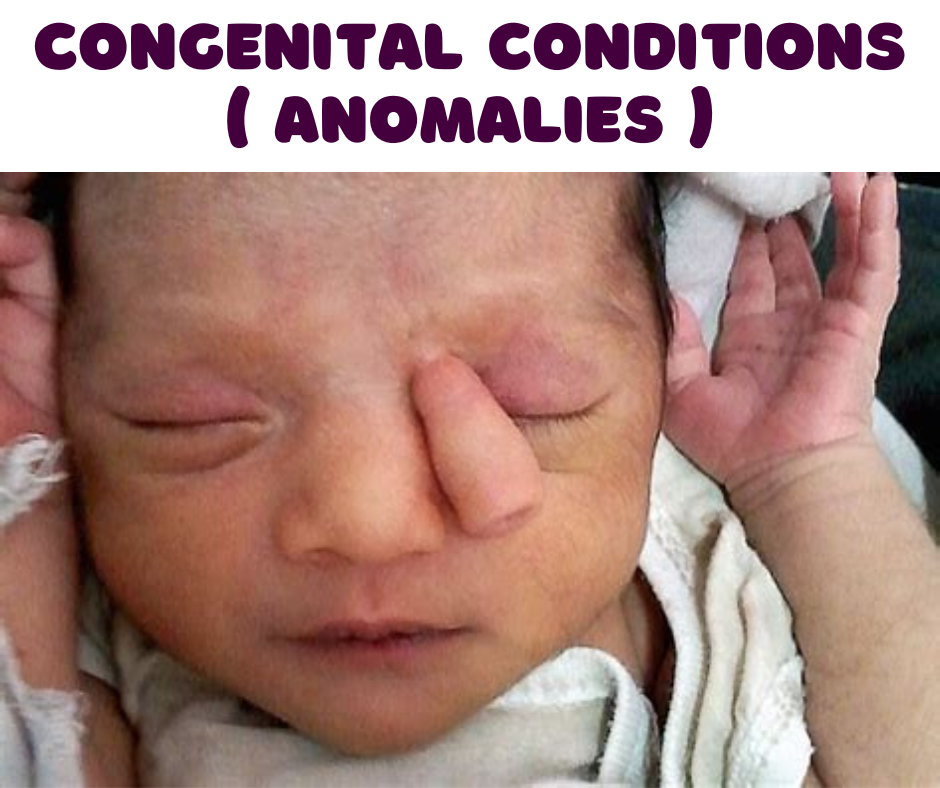
Congenital conditions, also referred to as congenital disorders, encompass a range of health issues present from birth. These conditions may arise from genetic abnormalities, environmental factors, or a combination of both, resulting in a diverse spectrum of manifestations that affect physical and mental development. Understanding congenital conditions is crucial in the field of medicine, as they profoundly influence individual health outcomes and family dynamics.
Approximately 3-5% of infants are born with congenital conditions, highlighting their significant prevalence. These conditions can vary widely in severity. Some are relatively mild and may not require intervention, while others can lead to major health challenges requiring comprehensive medical care. Common examples of congenital conditions include congenital heart defects, spina bifida, and Down syndrome, each characterized by distinct features and management strategies.
The formation of congenital conditions can occur during the embryonic or fetal stages of development. Genetic factors might trigger these abnormalities, leading to inherited conditions passed through generations. Alternatively, environmental exposures, such as maternal drug use, infections, or poor nutrition during pregnancy, can contribute to the development of certain disorders. Understanding the etiology of congenital conditions is essential for parents and healthcare professionals alike as it influences both preventive strategies and potential treatment options.
Moreover, the impact of congenital conditions extends beyond the individual. Families often face a range of emotional, financial, and social challenges. Awareness and education about these disorders play a critical role in supporting affected families and improving health outcomes. Overall, a comprehensive understanding of congenital conditions is imperative in recognizing their implications and designing effective management approaches for those affected.
Types of Congenital Conditions
Congenital conditions are classified into several categories based on their nature, etiology, and the systems they affect. Understanding these types helps in recognizing the diverse spectrum of congenital disorders, facilitating early diagnosis and management. The three major categories include structural defects, chromosomal conditions, and metabolic disorders.
Structural defects refer to physical abnormalities in organ or body structure, often resulting from disruptions during fetal development. One prominent example is congenital heart defects, which can range from simple issues like a small hole in the heart to complex abnormalities necessitating surgical intervention. Another common structural defect is a cleft palate, which occurs when there is an incomplete fusion of the lip and/or the roof of the mouth. These defects can have significant implications for the child’s health, function, and quality of life.
Chromosomal conditions arise from abnormalities in an individual’s chromosomes, leading to significant developmental and physical challenges. A well-known example is Down syndrome, where an extra copy of chromosome 21 results in characteristic physical features and intellectual disabilities. Other chromosomal disorders, such as Turner syndrome and Klinefelter syndrome, can affect sexual development and fertility, among other aspects of health.
Metabolic disorders represent another crucial type of congenital condition, resulting from enzyme deficiencies that disrupt normal metabolic processes. A prime example is phenylketonuria (PKU), a disorder characterized by the inability to metabolize phenylalanine, leading to severe intellectual disability if not managed through a strict diet. Detecting metabolic disorders promptly can be life-changing, as early management may prevent irreversible damage.
These categories of congenital conditions, encompassing structural defects, chromosomal disorders, and metabolic issues, illustrate the complexity and variety of congenital conditions. Understanding their types is vital for healthcare professionals and families navigating the challenges presented by these conditions.
Causes of Congenital Conditions
Congenital conditions, defined as disorders present at birth, can arise from a variety of factors. Understanding these causes is crucial for prevention and management strategies. Genetic factors are one of the primary contributors to congenital disorders. These can include single-gene mutations as well as chromosomal abnormalities, such as Down syndrome, which is caused by an extra chromosome. Hereditary conditions often have a familial pattern, indicating a genetic predisposition that can be assessed through family history.
Environmental influences play an equally significant role in the development of congenital conditions. Exposure to harmful substances during pregnancy can lead to various developmental issues. Maternal drug use, particularly with substances like alcohol, certain medications, and illicit drugs, has been strongly linked to congenital syndromes. Fetal Alcohol Spectrum Disorders (FASDs), for instance, result from alcohol consumption during pregnancy and can result in a range of lifelong effects on physical, cognitive, and behavioral development.
Moreover, exposure to environmental toxins, such as pesticides, heavy metals, and radiation, has been implicated in the manifestation of congenital disorders. The timing of exposure is crucial; certain critical periods during pregnancy may heighten vulnerability to these environmental factors. Additionally, lifestyle choices made by the mother during pregnancy, including poor nutrition, smoking, and lack of prenatal care, can exacerbate risks associated with congenital conditions.
The interaction between genetic factors and environmental influences is complex. For instance, an individual may have a genetic predisposition to a certain condition, but whether it manifests may depend on environmental triggers. Understanding these interconnections is essential for minimizing risk factors associated with congenital disorders, highlighting the importance of preventive care and early intervention in prenatal health.

Diagnosis of Congenital Conditions
Diagnosing congenital conditions is a critical aspect in managing overall health, as early detection can significantly improve outcomes for affected individuals. There are two primary phases of diagnosis: prenatal screening and postnatal evaluations. Prenatal screening typically involves various non-invasive techniques aimed at identifying potential congenital anomalies during pregnancy.
One of the most common methods used in prenatal screening is ultrasound imaging. This technique allows healthcare providers to visualize the developing fetus and assess its anatomy for any structural abnormalities. Ultrasounds can often detect conditions such as spina bifida, cleft lip, and other visible defects, usually performed during the first and second trimesters. Additionally, blood tests, including maternal serum screening and cell-free fetal DNA testing, can provide crucial information regarding the risk of chromosomal abnormalities, such as Down syndrome. These tests analyze specific markers in the mother’s blood to estimate the likelihood of these conditions, thereby enabling healthcare professionals to offer further diagnostic options if necessary.
Postnatal evaluations are essential for diagnosing congenital conditions that may not be apparent before or during birth. Healthcare providers conduct thorough physical examinations immediately after birth, looking for visible signs of congenital anomalies. If there are concerns, further diagnostic methods may include genetic testing, which analyzes chromosomes and genes to identify conditions that may not present physically. Genetic testing can be particularly useful in conditions with hereditary components, guiding treatment options and informing families about potential risks.
Early detection of congenital conditions through these diagnostic methods plays a pivotal role in ensuring timely management, which may include medical interventions, surgery, or ongoing monitoring, ultimately leading to better health outcomes for the affected individuals and their families.
Symptoms and Effects of Congenital Conditions
Congenital conditions, which are often present at birth, exhibit a wide range of symptoms that can vary significantly from one individual to another. These symptoms depend on the specific condition, its severity, and the systems affected within the body. Common symptoms may include physical anomalies, developmental delays, or functional impairments, highlighting the heterogeneity in presentation.
Among congenital heart defects, symptoms often manifest as difficulty in feeding, rapid breathing, and cyanosis, which denotes a bluish tint to the skin due to lack of oxygen. In contrast, conditions such as spina bifida may present with noticeable spinal deformities, neurological deficits, and issues with mobility. Similarly, congenital disorders affecting the metabolic processes can lead to lethargy, vomiting, or developmental regression during infancy. Recognizing these symptoms early can be pivotal for timely intervention and management.
The effects of congenital conditions can be both short- and long-term, influencing an individual’s overall quality of life. Short-term effects might include challenges in physical health, such as frequent hospital visits or the need for medications and interventions. As individuals grow, these symptoms can evolve, leading to long-term effects that may affect educational and occupational opportunities. For instance, those with conditions affecting vision or hearing might face significant barriers in academic settings, while others with chronic conditions may encounter challenges in maintaining employment.
Beyond physical health implications, emotional well-being is also impacted by congenital conditions. Individuals and families may experience feelings of anxiety, frustration, and grief related to the ongoing management of symptoms. Support networks and mental health resources can play a crucial role in mitigating these emotional challenges. Ultimately, understanding the spectrum of symptoms and their effects is essential for developing effective treatment plans and enhancing overall patient care.
Management and Treatment Options
Management and treatment options for congenital conditions are diverse and tailored according to the individual needs of each patient. A multidisciplinary approach is often the most effective, as many congenital disorders require the involvement of various healthcare professionals. This may include pediatricians, surgeons, physical therapists, occupational therapists, and speech therapists, among others. Each professional plays a crucial role in developing an individualized care plan designed to address the unique challenges posed by the specific congenital condition.
Surgery is often a primary treatment option for certain congenital conditions, especially those affecting the heart, limbs, or internal organs. Surgical intervention may be necessary to correct anatomical abnormalities, improve functionality, or alleviate symptoms. For example, congenital heart defects may require surgical repair to ensure normal blood circulation. The timing and type of surgery depend on the complexity of the condition and the patient’s overall health.
Beyond surgical options, various therapeutic interventions can also significantly enhance the quality of life for individuals with congenital conditions. Physical therapy focuses on improving mobility and physical function, which can be vital for children who face developmental delays or physical limitations. Occupational therapy assists patients in developing daily living skills, fostering independence. Speech therapy can be essential for those with congenital conditions affecting communication abilities, ensuring they can express themselves effectively.
In addition to therapeutic methods, medication may also be crucial for managing symptoms associated with congenital conditions. This could include pain management, antibiotics to prevent infections, or medications to regulate heart function in individuals with congenital heart disorders. The specific treatment plan will depend on the individual’s unique needs, and continuous assessment and adjustment are essential to optimize outcomes.
Ultimately, the individualization and integration of various treatment modalities reflect the complexities of managing congenital conditions. It is vital that families work closely with healthcare providers to ensure that care plans are effectively tailored to the patient’s specific circumstances and progress.

Living with a Congenital Condition
Individuals with congenital conditions face unique challenges that extend beyond their physical health. The journey begins at diagnosis and continues throughout their lives, often necessitating ongoing medical intervention and support. Mental health is a crucial aspect of living with these conditions, as individuals may experience feelings of isolation, anxiety, or depression due to their health circumstances. Proper mental health support, such as counseling or therapy, can be vital in helping those affected cope with the emotional and psychological aspects of their condition.
Moreover, navigating healthcare systems can be overwhelming for families managing a congenital condition. Accessing appropriate medical care requires understanding various specialists, treatment plans, and insurance options. Families must often advocate fiercely for their loved ones, ensuring they receive the necessary care and resources. Connection with healthcare practitioners who understand the complexities of congenital conditions can help ease this burden, providing reliable guidance and support throughout the healthcare journey.
Community support also plays a pivotal role in the lives of those affected by congenital conditions. Local support groups and organizations can offer invaluable resources, fostering connections among families sharing similar experiences. Such communities provide not only emotional support but also practical advice on managing various aspects of living with a congenital condition, from education to daily activities. By sharing stories and strategies, families can find encouragement and hope in their shared resilience.
In conclusion, living with a congenital condition presents numerous complexities, but with proper mental health support, effective navigation of healthcare systems, and strong community ties, individuals and families can foster a sense of empowerment and improve their quality of life. This multifaceted approach highlights the importance of not only addressing physical health needs but also prioritizing emotional wellbeing and the advantages of a supportive network.
Research and Future Directions
The field of congenital conditions is experiencing significant advancements, primarily due to breakthroughs in genetic research. Recent studies have illuminated the genetic underpinnings of various congenital disorders, revealing complex interactions between multiple genes and environmental factors. This new understanding is crucial for identifying the root causes of these conditions, thus paving the way for targeted interventions. One promising area of focus is gene therapy, which aims to correct or mitigate the effects of genetic anomalies. Early-stage clinical trials are exploring gene editing technologies, like CRISPR-Cas9, that may one day provide effective treatments for genetic disorders that were previously deemed untreatable.
In addition to genetic research, there has been a notable shift towards integrated care models that address the multifaceted needs of individuals with congenital conditions. This includes not just medical treatment, but also psychosocial support and resources for affected families. Ongoing studies aim to evaluate the effectiveness of these holistic approaches, emphasizing the importance of mental health and social integration in improving quality of life for patients.
Looking ahead, the future of managing congenital conditions appears promising. Innovations in prenatal screening and diagnostics are likely to enhance early detection, allowing for timely interventions that could change the course of these disorders. Furthermore, as research continues to uncover the links between genetics and congenital conditions, it may lead to new preventive measures, reducing the incidence of these diseases in future generations. Collaboration among researchers, clinicians, and patient advocacy groups will be crucial in driving forward this agenda. Overall, the continued exploration of genetic factors and the efficacy of emerging therapies are expected to significantly improve outcomes for affected individuals.
FAQs about Congenital Conditions
Congenital conditions, which are abnormalities present at birth, encompass a wide spectrum of health issues. Understanding such conditions is crucial, and addressing common questions can improve awareness and knowledge among families and the public.
What causes congenital conditions?
Congenital conditions can arise from various factors. Genetic mutations, environmental influences, and specific maternal health issues during pregnancy play pivotal roles. For example, exposure to harmful substances, certain infections, and pre-existing maternal conditions can increase the risk of these disorders. Furthermore, familial genetic predispositions may also contribute to the likelihood of a child being born with a congenital condition.
How are congenital conditions diagnosed?
Diagnosis typically occurs through screenings and genetic testing during pregnancy. Ultrasounds and blood tests can detect certain conditions before birth. After birth, pediatricians perform physical examinations and may recommend additional diagnostic tests, including imaging or genetic testing, to identify congenital abnormalities accurately.
What support resources are available for families?
Families dealing with congenital conditions can access numerous support resources. Organizations dedicated to specific conditions provide educational materials, support groups, and counseling services. Hospitals often have social workers who can assist families in navigating care options, financial aid, and community resources. Online forums and local support groups also foster connection among families facing similar challenges.
Are there common myths about congenital conditions?
Yes, several myths surround congenital conditions. A prevalent misconception is that they are solely inherited. While genetics can play a significant role, environmental factors often contribute as well. Another myth is that congenital conditions will invariably lead to severe disabilities; in reality, the severity and impact can vary widely among individuals. Addressing these myths is vital in promoting awareness and understanding.
Through this exploration of commonly asked questions, it is evident that increasing public knowledge and reducing misconceptions around congenital conditions is paramount for affected families.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

