What is Autoimmune Inner Ear Disease (AIED)?
Autoimmune Inner Ear Disease, commonly referred to as AIED, is a rare condition characterized by an inappropriate immune response that targets the inner ear structures. This disorder disrupts the auditory and vestibular functions of the ear, leading to significant hearing loss and balance issues. AIED can affect individuals differently, often manifesting with symptoms such as progressive sensorineural hearing loss, tinnitus, and feelings of dizziness or imbalance.
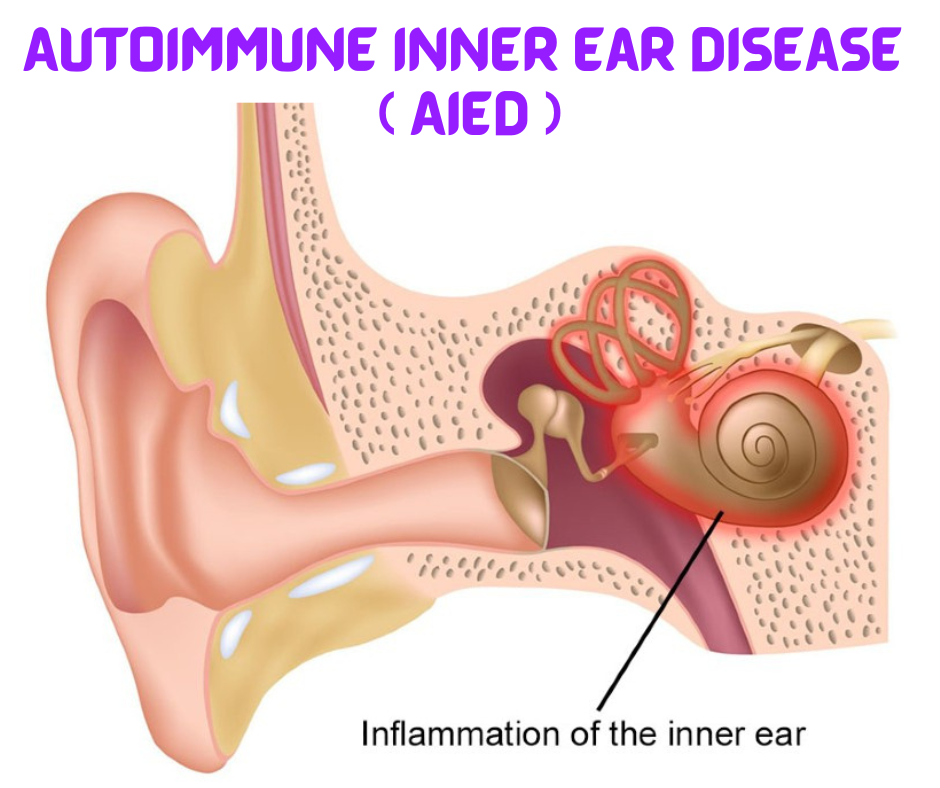
The underlying mechanism of AIED involves the body’s immune system mistakenly identifying inner ear tissues as threats. Usually, the immune system protects the body against harmful pathogens; however, in the case of AIED, the antibodies and immune cells aggressively attack the delicate structures of the inner ear. This immune response can result in inflammation and subsequent damage to the cochlea, the organ responsible for sound processing, as well as the vestibular system, which maintains balance.
From an audiological perspective, AIED is significant as it presents unique challenges for diagnosis and treatment. Patients often undergo extensive evaluation to distinguish AIED from other forms of hearing loss, such as noise-induced or age-related degeneration. Advanced imaging techniques and auditory assessments play essential roles in diagnosis, while clinicians must also consider the possible presence of other autoimmune disorders that may co-occur.
Understanding AIED is crucial for audiologists and healthcare professionals because early intervention can greatly influence patient outcomes. Treatments typically aim at dampening the immune response to preserve hearing and balance functions. Corticosteroids and immunosuppressive agents are commonly employed, reflecting the need for a tailored approach in managing this complex condition.
Causes and Risk Factors
Autoimmune Inner Ear Disease (AIED) is a complex condition characterized by the body’s immune system erroneously targeting the inner ear structures. Several potential causes and risk factors contribute to the development of AIED, which can be broadly categorized into genetic predispositions, environmental influences, and associations with other autoimmune disorders.
Genetic predispositions play a significant role in the likelihood of developing AIED. Certain individuals may inherit genes that increase susceptibility to autoimmune conditions. Familial tendencies have been observed, suggesting that a hereditary component may contribute to the likelihood of AIED. Individuals with a family history of autoimmune diseases may be at a higher risk, as genetic markers often correlate with an increased immune response.
Environmental factors can also influence the onset of AIED. Exposure to certain medications, infections, and toxins may trigger immune responses that target the inner ear. For instance, viral infections like Cytomegalovirus (CMV) and Epstein-Barr virus (EBV) have been implicated in the development of various autoimmune conditions, including AIED. Additionally, environmental elements such as heavy metals or chemical exposures can initiate autoimmune processes that lead to ear disease.
Moreover, demographic factors are relevant in understanding AIED. Research indicates that women are more frequently diagnosed with AIED than men, particularly in middle to late adulthood. Age is another crucial factor, with individuals typically affected between the ages of 40 and 60. Furthermore, the presence of other autoimmune conditions, such as lupus or rheumatoid arthritis, may increase the risk of developing AIED. These associations underline the multifaceted nature of AIED, where genetic, environmental, and demographic factors intertwine to influence disease onset and progression.
Symptoms of Autoimmune Inner Ear Disease
Autoimmune Inner Ear Disease (AIED) presents a range of symptoms that can vary significantly among individuals, often leading to complexities in diagnosis and management. The most predominant symptom associated with AIED is hearing loss, which may manifest as a gradual decline or a sudden change in auditory perception. This progressive loss is frequently bilateral, affecting both ears, although some individuals may initially experience unilateral symptoms. The degree of hearing impairment can fluctuate over time, making it challenging for patients to recognize the underlying condition.
Another common symptom of AIED is tinnitus, characterized by persistent ringing, buzzing, or hissing sounds in one or both ears. Tinnitus associated with AIED can vary in intensity and may exacerbate the perception of hearing loss. Many patients report that this symptom significantly impacts their quality of life, often leading to increased anxiety and difficulty concentrating.
In addition to hearing loss and tinnitus, individuals with AIED frequently encounter balance issues. The inner ear plays a crucial role in maintaining equilibrium, and inflammation associated with AIED can disrupt vestibular function, leading to dizziness, unsteadiness, or vertigo. Some patients may find that these balance disturbances contribute to falls or difficulties in performing daily activities.
It is essential to recognize that the symptoms of AIED can progress over time, often resulting in a worsening of auditory and vestibular functions. Here, variability is key: not every patient will present with all symptoms, and the progression can differ widely. Some may experience a more insidious decline, while others could have a rapid onset of symptoms that escalates quickly. Thus, awareness of these signs is critical for early detection and intervention in AIED.

Diagnosis of AIED
Diagnosing Autoimmune Inner Ear Disease (AIED) is a complex process that necessitates a comprehensive approach to differentiate it from other forms of hearing loss. The initial step often involves a thorough medical history and physical examination, followed by a series of audiometric tests. These tests measure a patient’s hearing ability and can help identify the specific type of hearing impairment present. In the case of AIED, typical findings may include fluctuating hearing loss, which is distinct from more common types of hearing issues.
One essential aspect in the diagnosis of AIED is the need for differential diagnosis. This process is crucial as AIED can mimic other conditions such as Meniere’s disease, vestibular schwannomas, or idiopathic sudden sensorineural hearing loss. To accurately define AIED, clinicians often employ imaging studies, such as Magnetic Resonance Imaging (MRI), to rule out structural abnormalities in the ear and central nervous system. These imaging techniques can provide visual confirmation of any underlying issues contributing to the hearing loss.
Additionally, laboratory tests play a significant role in diagnosing autoimmune disorders. Blood tests are conducted to assess for specific autoimmune markers. Physicians typically look for markers such as antinuclear antibodies (ANA) or other immunological profiles that may indicate an autoimmune response affecting the inner ear. The presence of such markers can provide instrumental support for an AIED diagnosis, especially when other potential causes have been excluded.
In summary, diagnosing AIED involves a combination of audiometric evaluations, imaging studies, and laboratory analyses. These methods not only confirm the presence of hearing loss but also help distinguish AIED from other conditions that may cause similar symptoms. A well-rounded diagnostic approach is paramount to ensure accurate identification and treatment of this complex disorder.
Common Treatments and Management Strategies
For individuals diagnosed with Autoimmune Inner Ear Disease (AIED), a variety of treatment options are available aimed at managing symptoms and improving quality of life. The cornerstone of AIED treatment often involves pharmacological interventions, most notably corticosteroids. These medications serve to reduce inflammation within the inner ear, thereby helping to preserve hearing and mitigate other auditory symptoms associated with the condition. Corticosteroids can be administered orally or through injections based on the severity and progression of the disease.
In some cases, if corticosteroids alone are not effective or if the patient experiences adverse effects, immunosuppressants may be considered. Drugs such as methotrexate or mycophenolate mofetil can help dampen the immune response that contributes to the inner ear damage seen in AIED. This therapeutic approach aims to stabilize hearing and prevent further deterioration, although it requires careful monitoring due to potential side effects and the need for regular blood tests to ensure patient safety.
Apart from pharmaceutical treatments, lifestyle modifications play a crucial role in the management of AIED. Patients are often advised to engage in a balanced diet rich in anti-inflammatory foods, stay well-hydrated, and limit exposure to noise to reduce stress on the auditory system. Incorporating stress-reduction techniques such as yoga or meditation can also be beneficial in managing the overall health and well-being of individuals with AIED.
Additionally, therapeutic interventions such as hearing aids and counseling can provide significant support for those experiencing hearing loss or related emotional challenges. Hearing aids can enhance communication ability, while counseling can help individuals cope with the psychological aspects of living with a chronic health condition. By adopting a comprehensive approach that combines medical treatment with lifestyle adjustments and supportive therapies, individuals diagnosed with AIED can better manage their symptoms and maintain a higher quality of life.
Living with Autoimmune Inner Ear Disease
Living with Autoimmune Inner Ear Disease (AIED) presents a unique set of challenges that extend beyond the physical symptoms. Individuals diagnosed with AIED often experience a significant emotional and mental toll due to the unpredictable nature of the condition. This chronic illness can lead to feelings of isolation, anxiety, and depression as patients navigate through fluctuating hearing loss and balance issues. Acknowledging and addressing these emotional aspects is crucial for managing the overall well-being of those affected by AIED.
Coping strategies play a vital role in enhancing the quality of life for individuals with AIED. Engaging in activities that promote relaxation, such as meditation or gentle exercise, can help reduce stress and anxiety. Additionally, maintaining open communication with family and friends fosters a supportive environment. This network of support can be instrumental in providing encouragement and understanding, which is essential for emotional resilience. Finding support groups—either in-person or online—can connect individuals with others who share similar experiences, allowing for the exchange of coping strategies and emotional support.
Furthermore, access to resources tailored to those with hearing and balance challenges can aid in daily life. Audiologists and speech therapists can provide personalized rehabilitation exercises, which may improve communication skills. Technology, such as hearing aids and assistive listening devices, can also significantly enhance auditory experiences, helping individuals engage more fully in their daily activities. Education about the disease is another essential resource, empowering patients with knowledge about their condition and available treatment options. By actively seeking out these resources, individuals can reclaim agency over their health and enhance their coping mechanisms in the face of AIED.

Recent Research Developments in AIED
Autoimmune Inner Ear Disease (AIED) has garnered significant attention in recent years, leading to advances in our understanding of the immune system’s role in ear-related disorders. Researchers are uncovering intricate mechanisms that explain how immune responses can target inner ear tissue, ultimately resulting in profound hearing loss. One of the breakthroughs has been the identification of specific autoantibodies that may serve as biomarkers for AIED, enabling earlier and more accurate diagnosis.
In current studies, scientists are investigating how the immune system interacts with the delicate structures of the inner ear. This interaction can be detrimental, as the body may mistakenly attack its own ear tissues, leading to inflammation and damage. Recent findings suggest that certain cytokines and chemokines participate in this pathological process, highlighting prospects for targeted therapies that can modulate immune responses without compromising the overall immune function.
Novel treatments are also on the horizon. Researchers are exploring the potential of biologic therapies that could inhibit the specific immune pathways involved in AIED. These therapies, which are already used in other autoimmune conditions, hold promise for mitigating the progression of the disease and possibly restoring hearing function. Furthermore, clinical trials are being conducted to evaluate the efficacy of immunomodulatory agents, with early results indicating encouraging outcomes for improvement in auditory function.
Technological advancements also play a key role in the future of AIED management. For instance, digital otoscopy and imaging techniques are enhancing our ability to visualize inner ear structures and monitor disease progression non-invasively. Additionally, emerging artificial intelligence (AI) applications are being designed to analyze patient data, improving diagnostic accuracy and personalizing treatment plans. These exciting developments symbolize a movement toward a more nuanced and effective approach to understanding and managing AIED.
Frequently Asked Questions (FAQs)
Autoimmune Inner Ear Disease (AIED) is a complex condition that often raises numerous questions among those affected and their families. Understanding AIED is crucial for effective management and coping strategies. Below are some of the most frequently asked questions about this condition.
What is the prevalence of AIED?
AIED is considered rare, affecting approximately 1 in 10,000 individuals. While its exact prevalence is not fully established, it is often underdiagnosed or misdiagnosed, leading to an underrepresentation of actual cases in clinical studies and statistics.
How effective are treatments for AIED?
Treatment efficacy can vary significantly among individuals. Corticosteroids are commonly prescribed to manage inflammation and slow disease progression. Some patients may experience marked improvement, while others may notice little change. Other therapies, such as immunosuppressive drugs, may also be explored, particularly for cases resistant to steroid treatment.
What is the long-term prognosis for individuals with AIED?
The long-term prognosis for AIED varies widely. Some individuals may maintain a stable level of hearing over time, while others face progressive hearing loss. Regular monitoring and proactive management strategies can mitigate potential complications, making early diagnosis crucial in improving outcomes.
Are there lifestyle adjustments that may benefit those with AIED?
Yes, individuals with AIED can optimize their health through several lifestyle modifications. A balanced diet rich in anti-inflammatory foods, regular exercise, and stress management techniques such as yoga or meditation can contribute positively to overall well-being. It is also advisable to avoid loud noises and limit exposure to ototoxic medications whenever possible.
What are the common symptoms of AIED?
The symptoms of Autoimmune Inner Ear Disease (AIED) can vary greatly among individuals but typically include sudden or fluctuating hearing loss, tinnitus (ringing in the ears), dizziness, and balance issues. These symptoms may appear in one or both ears and can sometimes be mistaken for other ear conditions. Early recognition of these symptoms is important for prompt treatment and management.
Addressing these questions can help demystify AIED, empowering individuals affected by this condition with knowledge and support as they navigate their journeys.
Conclusion and Future Perspectives
Autoimmune Inner Ear Disease (AIED) remains a complex and multifaceted condition characterized by hearing loss and balance issues stemming from the immune system attacking the inner ear structures. Key symptoms include progressive hearing loss, tinnitus, and sometimes vertigo, which collectively underscore the importance of early and accurate diagnosis. Physicians often utilize a combination of clinical history, audiometric testing, and advanced imaging techniques to differentiate AIED from other causes of hearing impairment. This is a crucial step, as timely intervention can significantly influence outcomes for patients.
Current treatment protocols primarily focus on immunosuppressive therapies, including corticosteroids, which have demonstrated efficacy in managing AIED symptoms. However, the variability in patient responses highlights the need for tailored treatment strategies. As research continues, a deeper understanding of the underlying autoimmune processes involved in AIED may lead to more effective and personalized therapeutic options. Ongoing studies are exploring novel immunomodulatory agents, which could potentially offer benefits over traditional corticoid treatments, aiming to minimize side effects and enhance patient quality of life.
Looking toward the future, it is imperative that the medical community maintains a focus on comprehensive research initiatives that investigate both the pathophysiology of AIED and patient-centered approaches to treatment. Collaboration between audiologists, immunologists, and other specialists will be essential in developing a multidisciplinary approach that addresses the diverse needs of AIED patients. Furthermore, increased awareness and education among healthcare providers and patients about this condition can facilitate earlier diagnosis and intervention. The ultimate goal is to improve therapeutic outcomes, ensuring that patients with AIED lead fulfilling lives, with greater hearing preservation and overall health.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

