Benign Paroxysmal Positional Vertigo: 5 Dark Signs
What is Benign Paroxysmal Positional Vertigo?
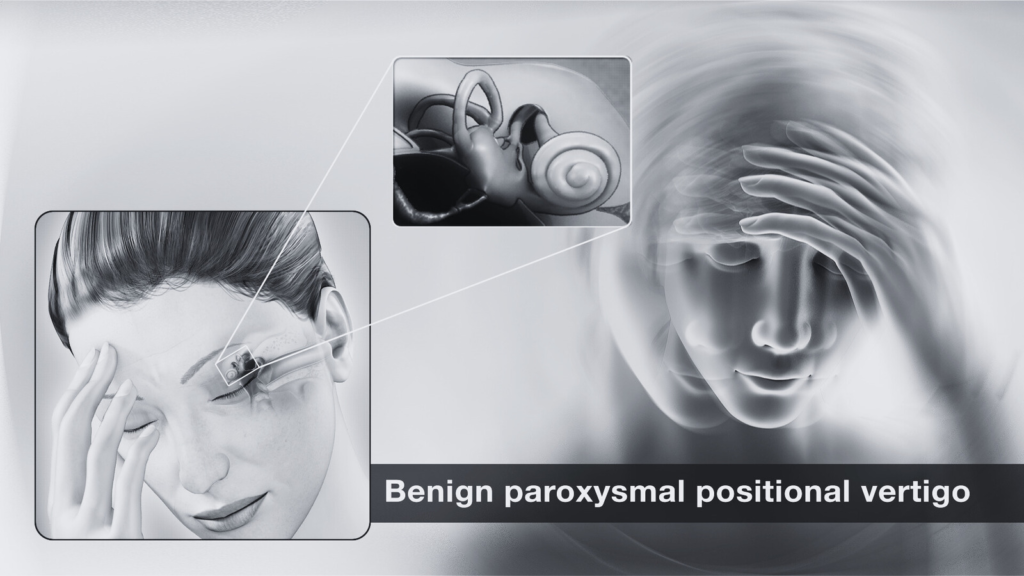
Benign Paroxysmal Positional Vertigo, commonly referred to as BPPV, is a prevalent vestibular disorder that is recognized as one of the leading causes of dizziness. The condition is characterized by episodes of vertigo that typically occur with changes in the position of the head. Specifically, BPPV affects the inner ear, where the vestibular system resides. This crucial system is responsible for maintaining balance and spatial orientation.
The term “benign” is essential in understanding BPPV, as it indicates that the condition, while distressing, is not life-threatening. This distinction is particularly significant for individuals experiencing the distressing symptoms of dizziness and imbalance, as it provides reassurance that the underlying causes are not severe in nature. BPPV is caused by the displacement of tiny calcium carbonate crystals, known as otoconia, within the semicircular canals of the inner ear. When these crystals become dislodged and move into one of the canals, they can interfere with the normal fluid movement that helps the body recognize head position and balance.
As a result, individuals with BPPV may experience brief but intense episodes of vertigo, often triggered by specific head movements, such as turning over in bed or looking up. Alongside dizziness, individuals may also report symptoms such as nausea, imbalance, and even unsteadiness while walking. Understanding the mechanics of BPPV is essential for both patients and healthcare professionals, as it plays a significant role in diagnosing and treating the condition effectively.
Causes of BPPV
Benign Paroxysmal Positional Vertigo (BPPV) is primarily caused by the dislodgment of otoconia, which are tiny calcium carbonate crystals located in the inner ear. Under normal circumstances, these otoconia help maintain balance and spatial orientation. However, when they become dislodged from their usual position and migrate into the semicircular canals of the inner ear, they can lead to episodes of vertigo, which are characterized by a false sensation of spinning or movement. This disruption in the vestibular system is a crucial factor in the development of BPPV.
Several factors can trigger the dislodgment of otoconia, and among the most common is head trauma. A significant impact to the head, whether from a fall or an accident, can cause these crystals to displace and become lodged inappropriately. Age-related degeneration is another significant risk factor; as individuals age, the fluids and structures of the inner ear can undergo changes that increase the likelihood of otoconia becoming loose. This is particularly relevant for those over the age of 50, who are statistically more vulnerable to experiencing episodes of BPPV.
Additionally, prolonged bed rest or inactivity is another factor that may predispose individuals to this condition. When a person remains in a recumbent position for an extended period, the otoconia may detach more easily. Other potential triggers for BPPV include certain ear diseases, vestibular disorders, and even surgical interventions affecting the inner ear. Understanding these causes is essential for identifying susceptibility to BPPV and helps raise awareness about this commonly misunderstood disorder.
Symptoms of Benign Paroxysmal Positional Vertigo
Benign Paroxysmal Positional Vertigo (BPPV) is primarily characterized by brief episodes of vertigo that are triggered by specific changes in head position. Individuals afflicted with BPPV often experience a spinning sensation when they turn their heads, tilt their heads backward, or lie down. This sensation is typically described as a feeling that the surroundings are spinning, leading to disorientation and dizziness that may last anywhere from a few seconds to a couple of minutes. The duration and intensity of these episodes can vary widely among individuals, and they may occur sporadically or in clusters.
Alongside the distinctive spinning sensation, patients may also experience additional symptoms that can complicate their condition. Nausea is a common accompanying feature, as the conflicting signals between the inner ear and the eyes can lead to a feeling of discomfort. In some cases, individuals may experience imbalance, which can result in difficulty walking or standing, elevating the risk of falls. It is important to note that these episodes can induce anxiety, especially when they occur unexpectedly in public or stressful scenarios. This anxiety may further exacerbate the sensation of dizziness, creating a cycle that can be challenging to break.
Furthermore, symptoms might become more pronounced when the individual is positioned in bed or when attempting certain activities that require head movement. It is crucial for individuals to recognize these hallmark symptoms of BPPV, as early identification can facilitate appropriate management and treatment. Seeking medical advice is recommended for anyone experiencing sudden or persistent vertigo episodes, as accurate diagnosis can lead to effective interventions and improved quality of life.

Diagnosis of BPPV
The diagnosis of Benign Paroxysmal Positional Vertigo (BPPV) primarily relies on a comprehensive clinical evaluation conducted by a healthcare provider. During the initial consultation, the clinician will take a detailed medical history, focusing on the patient’s symptoms, including episodes of vertigo triggered by specific head positions. The characteristic nature of these episodes typically helps in recognizing the condition.
One of the key physical examination techniques employed in the diagnosis of BPPV is the Dix-Hallpike maneuver. This test is designed to provoke symptoms and identify which ear may be affected. During the maneuver, the healthcare provider will ask the patient to quickly turn their head to one side while being tilted backward at a 45-degree angle. This action helps in assessing the presence of nystagmus—a rapid, involuntary eye movement common in BPPV. Observation of the patient’s eye movements during this test can provide critical information for the correct diagnosis.
In addition to the Dix-Hallpike maneuver, thorough evaluations may require the use of imaging tests like MRI or CT scans, although these are generally not the first step in diagnosing BPPV. Imaging is typically reserved for cases where the clinician suspects a more serious underlying condition, such as a central vestibular lesion. The healthcare provider may recommend these tests if the vertigo episodes are atypical or if the patient has additional neurological signs that warrant further exploration. Understanding the diagnostic process arms the patient with knowledge about what to expect when visiting a healthcare provider with suspected BPPV, thus alleviating some anxiety associated with the clinical evaluation.
Treatment Options for BPPV
The management of Benign Paroxysmal Positional Vertigo (BPPV) largely revolves around repositioning maneuvers, lifestyle adjustments, and medications aimed at symptom relief. Central to the treatment of BPPV are canalith repositioning maneuvers, among which the Epley maneuver is the most frequently utilized. This procedure involves a series of specific head and body movements designed to relocate dislodged otoliths from the semicircular canals back into the utricle, where they can no longer cause vertigo. The Epley maneuver has demonstrated high efficacy rates, often providing immediate symptom relief during a single session.
In addition to the Epley maneuver, there are alternative canalith repositioning techniques such as the Semont maneuver and the Brandt-Daroff exercises. The Semont maneuver, like the Epley, aims to reposition the particles causing the sensation of spinning, while Brandt-Daroff exercises can be performed at home to help alleviate symptoms through repeated motion. These exercises provide patients with an active role in their recovery, often enhancing the treatment experience.
Lifestyle modifications also play a significant role in managing BPPV symptoms. Patients are encouraged to avoid specific head movements that may trigger vertigo episodes and to implement safety measures, such as removing trip hazards, to prevent falls during episodes of dizziness. Hydration and adequate rest are essential, as fatigue and dehydration may exacerbate symptoms. Even though medications, such as antihistamines, may be prescribed to alleviate acute symptoms, they are generally considered adjuncts rather than primary treatments, as they do not address the underlying cause of BPPV.
In conclusion, the treatment options for BPPV vary widely, covering maneuver-based therapies, lifestyle adjustments, and supportive medications. By employing a combination of these strategies, patients can effectively manage their symptoms and greatly improve their quality of life.
Managing BPPV at Home
Managing Benign Paroxysmal Positional Vertigo (BPPV) at home can significantly enhance the quality of life for individuals affected by this condition. The symptoms of BPPV, primarily characterized by episodes of intense dizziness triggered by changes in head position, can often be mitigated with proactive measures and adjustments in daily routines.
One of the most effective strategies for managing BPPV involves the application of certain head positioning techniques. The Epley maneuver, for instance, can be particularly beneficial. This repositioning method helps to relocate the displaced otoliths (tiny calcium carbonate crystals) back to their original location in the inner ear, thereby alleviating symptoms. Individuals can learn and practice this technique at home; however, it is essential to follow guidance from a healthcare practitioner to ensure correct execution.
In addition to repositioning exercises, individuals should also be mindful of their environment to reduce the risk of vertigo triggers. Maintaining a clutter-free living space can help prevent accidents caused by sudden dizziness. Furthermore, using non-slip mats, ensuring proper lighting, and installing grab bars in critical areas like bathrooms can enhance safety. It is important to inform family members or caretakers about one’s condition so they can provide support when needed.
Lastly, hydration and proper nutrition can play a role in managing vertigo symptoms. Staying well-hydrated can ensure optimal bodily function, while avoiding excessive caffeine and alcohol may help minimize dizziness. Keeping a journal to track potential triggers can also empower individuals. By identifying patterns and specific movements or circumstances that lead to vertigo episodes, one can implement more effective preventive measures.
By integrating these home management strategies, individuals with BPPV can take significant steps towards controlling their symptoms while also maintaining open communication with medical professionals for ongoing management and support.

Frequently Asked Questions (FAQs) about BPPV
Benign Paroxysmal Positional Vertigo (BPPV) often raises several questions among those affected by it. Understanding the condition can help ease concerns and clarify misconceptions.
What is the long-term outlook for individuals with BPPV?
The prognosis for BPPV is generally positive. Most individuals experience episodes that are brief and can be effectively treated. Treatment options, such as the Epley maneuver, often yield significant improvements. However, while BPPV can resolve quickly, some individuals may experience recurrent episodes throughout their lives. Regular follow-ups with a healthcare provider can aid in managing these episodes and monitoring overall health.
Is there a possibility of recurrence of BPPV?
Yes, recurrence is a common aspect of BPPV. Some studies indicate that approximately 50% of patients may experience a second episode within five years of their initial diagnosis. Certain factors, such as age and underlying vestibular disorders, may increase the likelihood of these recurrences. Being aware of one’s specific risk factors is important for managing expectations and seeking timely treatment.
What preventive measures can reduce the risk of BPPV?
While not all cases of BPPV can be prevented, certain measures may minimize the risk of future occurrences. These include maintaining a safe home environment to reduce fall risk, practicing vestibular rehabilitation exercises, and avoiding rapid head movements. Staying physically active and engaging in balance training can also help fortify the vestibular system, potentially lowering the risk of BPPV.
When should one seek medical help for BPPV?
It is advisable to seek medical assistance if you experience recurrent episodes of vertigo, especially if they are accompanied by additional symptoms such as nausea, vomiting, or hearing changes. Consulting a healthcare provider can ensure an accurate diagnosis and appropriate management of symptoms, helping to differentiate BPPV from other vestibular disorders.
Can BPPV affect both ears?
Yes, BPPV can affect one or both ears, though it more commonly occurs in just one. When both ears are involved, symptoms may be more persistent and challenging to treat. A healthcare professional can determine which ear is affected and recommend the most effective repositioning maneuvers accordingly.
Are there any lifestyle changes that can help manage BPPV?
Yes, certain lifestyle adjustments can help manage BPPV and reduce the frequency of episodes. These include sleeping with your head slightly elevated, avoiding sudden head movements, and being cautious when tilting your head backward or changing positions quickly. If you notice specific triggers, modifying your daily activities to minimize exposure to them can also be beneficial.
Evolution of Understanding BPPV
Benign Paroxysmal Positional Vertigo (BPPV) is a vestibular disorder characterized by episodes of dizziness associated with specific changes in head position. Historical accounts suggest that awareness of vertigo may date back to ancient civilizations, but it was not until the late 19th century that BPPV began to be distinctly recognized in medical literature. Initial descriptions of BPPV focused on its episodic nature and the relationship between head movements and the onset of symptoms.
The first significant advancements in understanding BPPV emerged in the mid-20th century. In 1952, Dr. Robert Barany published groundbreaking work that laid the foundation for diagnosing vestibular disorders, including BPPV. He elucidated the role of the inner ear, particularly the semicircular canals, which play a crucial role in balance and spatial orientation. Building upon Barany’s findings, researchers began to explore the mechanisms behind BPPV, leading to the identification of otoconia—tiny calcium carbonate crystals that, when displaced from their usual location in the utricle, can cause the vertiginous spells characteristic of BPPV.
In the decades that followed, diagnostic criteria for BPPV evolved significantly. With the advent of advanced imaging techniques and vestibular testing, clinicians gained the tools necessary for accurate identification of the condition. Recent research has also highlighted the importance of differentiating BPPV from other vestibular disorders, ensuring that patients receive appropriate treatment. Treatment approaches have progressed from simple repositioning maneuvers, such as the Epley maneuver, to more sophisticated therapeutic strategies encompassing personalized rehabilitation protocols.
This ongoing research and clinical observation continue to enhance the understanding of BPPV, guiding practitioners toward more effective interventions and improving patient outcomes. The historical context of BPPV illustrates an evolution from vague descriptions of dizziness to a well-defined clinical entity, recognizing its mechanical basis and refining diagnostic and treatment methodologies.
Conclusion: The Path Forward
In conclusion, understanding Benign Paroxysmal Positional Vertigo (BPPV) is vital for managing its impact on daily life. Throughout this blog post, we have explored the essential aspects of BPPV, including its causes, symptoms, and available treatments. BPPV primarily results from disturbances in the inner ear, where the displacement of tiny calcium carbonate crystals leads to episodes of vertigo triggered by specific head movements. Recognizing these symptoms is the first step toward effective management.
Diagnosis and treatment are critical in mitigating the distressing symptoms associated with BPPV. A comprehensive evaluation by a healthcare professional is necessary for confirming the diagnosis, as the condition can often be mistaken for other types of dizziness. Once diagnosed, patients can benefit from specialized treatments such as the Epley maneuver or other positional therapy techniques designed to reposition the displaced crystals within the inner ear.
Management strategies are essential for those experiencing recurring episodes of vertigo. In addition to therapeutic maneuvers, lifestyle modifications and exercises may significantly reduce the frequency and severity of symptoms, thus empowering individuals to regain control over their lives. Furthermore, ongoing advancements in the understanding of BPPV continue to emerge, leading to improved treatment protocols and better outcomes for patients.
It is important to remember that while BPPV can be alarming due to its sudden onset and the sensations it evokes, effective treatment options are readily available. By working closely with healthcare providers and adhering to recommended management strategies, individuals can navigate BPPV effectively and maintain their quality of life.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

