Brain Aneurysms: 7 Alarming Signs You Must Know
What is a Brain Aneurysm?
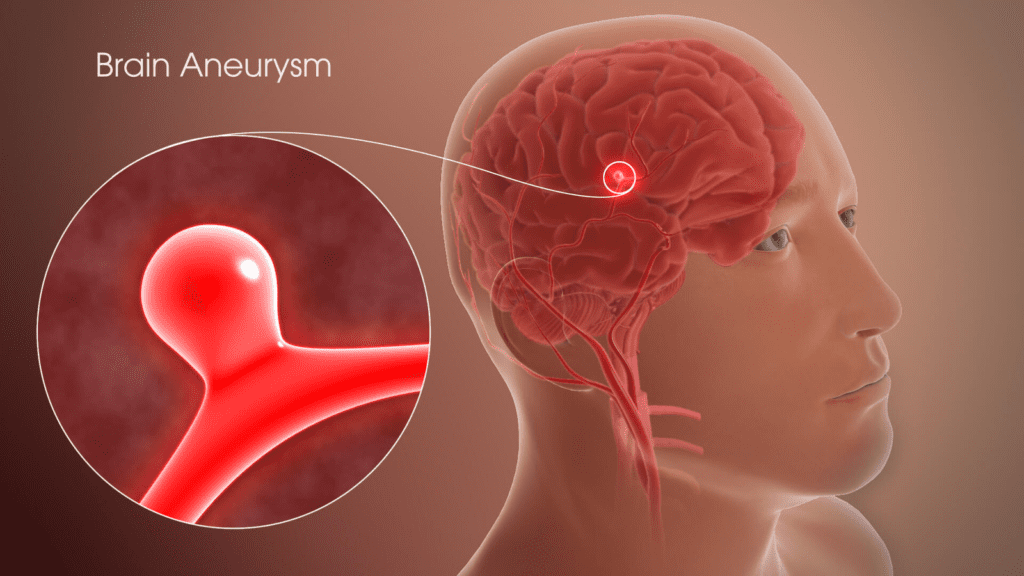
A brain aneurysm, also known as a cerebral aneurysm, is a localized dilation or bulge in the wall of a blood vessel in the brain. This condition occurs when the arterial wall becomes weakened, allowing it to stretch and form a sac-like structure filled with blood. Unlike systemic aneurysms that may occur in areas such as the aorta or peripheral arteries, a brain aneurysm specifically pertains to vessels within the cranial cavity.
The anatomy of the brain is composed of various types of blood vessels: arteries, veins, and capillaries. Arteries are responsible for delivering oxygen-rich blood from the heart to the brain, while veins return deoxygenated blood back to the heart. The formation of a brain aneurysm is often linked to congenital factors, hypertension, and other vascular conditions that contribute to the weakening of the arterial walls. Over time, the stressed blood vessel can give rise to abnormal ballooning, putting pressure on surrounding brain tissues and structures.
It is important to differentiate between a brain aneurysm and other forms of aneurysms. While cerebral aneurysms affect blood vessels in the brain, other types of aneurysms, such as aortic aneurysms, can occur in major arteries elsewhere in the body. The distinction is significant in terms of treatment approaches and potential complications. Brain aneurysms can lead to serious consequences if they rupture, resulting in a subarachnoid hemorrhage, which can cause life-threatening conditions or neurological deficits. Therefore, understanding the nature and specific characteristics of brain aneurysms is essential for both medical professionals and individuals at risk.
Types of Brain Aneurysms
Brain aneurysms, also known as cerebral aneurysms, can be classified into several distinct types, each with unique characteristics and formation processes. The three primary types include saccular, fusiform, and mycotic aneurysms. Understanding these variations is crucial for their diagnosis and treatment.
The most common type is the saccular aneurysm, which resembles a berry hanging on a stem. This type usually forms at the bifurcations of arteries, where the vessel wall is naturally weaker. Saccular aneurysms can vary in size and are often located in the anterior circulation of the brain. They account for approximately 80-90% of all brain aneurysms and can be asymptomatic; however, they pose a significant risk of rupture, leading to subarachnoid hemorrhage.
Fusiform aneurysms are larger and have a more diffuse appearance, involving the entire circumference of the artery rather than forming a distinct sac. These aneurysms arise from the degeneration of the arterial wall and are less prevalent, constituting only about 5-10% of cerebral aneurysms. They commonly occur in the vertebrobasilar circulation and can lead to various complications, including stenosis, which is a narrow formation in the artery that hinders blood flow.
Mycotic aneurysms are a rare but significant type caused by infection in the arterial wall, often stemming from systemic infections like endocarditis. This type can occur at any location within the cerebral vasculature and is characterized by its tendency to rupture more readily than other types due to compromised vessel integrity. Mycotic aneurysms account for less than 1% of brain aneurysms and require prompt medical intervention.
Each type of brain aneurysm presents its own risk factors and prevalence, highlighting the importance of early detection and appropriate treatment strategies for those affected.
Causes and Risk Factors
Brain aneurysms can arise from a variety of causes and risk factors that predispose individuals to their development. Understanding these factors is crucial for early detection and prevention strategies. Genetic predispositions play a significant role, as certain inherited conditions may increase the likelihood of aneurysm formation. Disorders such as Ehlers-Danlos syndrome, polycystic kidney disease, and von Willebrand disease are associated with a higher propensity for aneurysms and are often passed down through families.
Lifestyle factors also contribute significantly to the risk of developing a brain aneurysm. Smoking is a well-documented risk factor; the chemicals in tobacco can damage blood vessels, making them more susceptible to bulging and rupturing. Similarly, high blood pressure, or hypertension, is another critical contributor, as it places added strain on blood vessel walls, thereby increasing vulnerability. Reducing smoking rates and managing blood pressure through lifestyle changes and medication can potentially mitigate these risks.
Other medical conditions may also elevate the risk of brain aneurysms. Atherosclerosis, a condition characterized by the buildup of plaque in arteries, can weaken blood vessels and make aneurysm formation more likely. Furthermore, individuals with a history of head trauma may face a greater risk, as such injuries can compromise vascular integrity. Additionally, factors such as age and gender are noteworthy; the likelihood of developing an aneurysm increases with age, and women are generally at higher risk than men.
In conclusion, recognizing the causes and risk factors associated with brain aneurysms is essential for understanding their complexities. By acknowledging genetic, lifestyle, and medical contributors, individuals can take proactive steps in managing their health and reducing the risks associated with brain aneurysms.

Symptoms of Brain Aneurysms
Brain aneurysms, though often asymptomatic when unruptured, can present a myriad of signs and symptoms that vary depending on whether they have ruptured or not. It is crucial to differentiate these symptoms, as early recognition can be pivotal in seeking timely medical intervention.
An unruptured brain aneurysm might not exhibit overt symptoms; however, when symptoms do occur, they may include localized headaches, vision impairment, and changes in speech. Individuals may also experience discomfort behind the eye or a vague sense of pressure. These manifestations often emerge slowly and may be mistaken for benign conditions. As a result, the subtlety of these symptoms can lead many individuals to overlook them, emphasizing the need for medical evaluation if such signs persist.
On the other hand, a ruptured brain aneurysm can lead to severe and acute symptoms that demand immediate medical attention. The hallmark symptom is an extremely sudden and debilitating headache, often described as the “worst headache of one’s life.” This may be accompanied by nausea, vomiting, sensitivity to light, and a stiff neck. In some cases, individuals might also experience seizures or a sudden loss of consciousness. Furthermore, ruptured aneurysms can result in neurological deficits such as difficulty speaking or weakness on one side of the body, indicating a potential stroke.
Recognizing these symptoms is critical not only for individuals but also for healthcare professionals who may encounter patients presenting these signs. Prompt diagnosis and treatment can significantly enhance outcomes and potentially save lives. Therefore, awareness of both unruptured and ruptured brain aneurysm symptoms remains an integral aspect of managing this serious health condition.
Diagnosis of Brain Aneurysms
The diagnosis of brain aneurysms is a critical step in preventing potential complications, such as rupture and subsequent hemorrhagic stroke. Various imaging techniques are employed to visualize the brain’s vascular structures and identify the presence of aneurysms. The most common diagnostic tools include computed tomography (CT) scans, magnetic resonance imaging (MRI), and cerebral angiograms.
CT scans are widely used due to their speed and accessibility. In cases of a suspected rupture, a CT scan can quickly reveal the presence of blood in the subarachnoid space, indicating a possible aneurysm. However, for more detailed imaging of the blood vessels, MRI may be preferred. MRIs provide higher-resolution images and are particularly useful for visualizing smaller or unruptured aneurysms that may be missed during a CT scan.
Cerebral angiography is considered the gold standard for diagnosing brain aneurysms. This invasive procedure involves the use of a contrast dye injected into the bloodstream, allowing for real-time imaging of cerebral arteries. Angiograms provide precise information regarding the size, shape, and location of an aneurysm, facilitating treatment planning.
In addition to imaging techniques, neurological exams play a vital role in the diagnostic process. A physician will assess the patient’s history, symptoms, and perform a physical examination to evaluate neurological function. This information aids in determining the need for further diagnostic imaging. Moreover, family history can also contribute insight into an individual’s risk profile for developing brain aneurysms, as genetic factors may predispose certain individuals to such vascular malformations.
Overall, a multidisciplinary approach involving imaging techniques, neurological assessments, and consideration of family medical history is essential for accurate diagnosis and effective management of brain aneurysms.
Treatment Options for Brain Aneurysms
Brain aneurysms, characterized by a weakened area in a blood vessel wall, may require treatment depending on their size, location, and the patient’s health. Various treatment options are available, ranging from minimally invasive techniques to more traditional surgical procedures. The choice of treatment largely depends on a delicate balance between potential benefits and associated risks.
Surgical clipping is one of the most traditional approaches. This procedure involves opening the skull and placing a metal clip at the base of the aneurysm, effectively preventing blood flow into the aneurysm and reducing the risk of rupture. While clipping can be effective, it requires neurosurgery and carries risks, including infection, neurological damage, and complications related to anesthesia.
Another common method is endovascular coiling. This minimally invasive procedure involves threading a catheter through the blood vessels to the site of the aneurysm. Once there, tiny coils are deployed into the aneurysm to promote blood clotting and seal it off. Coiling has a shorter recovery time and a lower overall complication rate compared to clipping. However, it may not be suitable for all aneurysm types, particularly larger ones where flow diversion techniques may be more appropriate.
Flow diversion involves the placement of a stent-like device within the artery leading to the aneurysm. This option diverts blood flow away from the aneurysm, allowing it to shrink over time. Although it is a revolutionary approach, there may be a risk of complications, including ischemia or delayed rupture. Physicians may also opt for a watchful waiting approach for certain small, asymptomatic aneurysms, monitoring them regularly to determine if any changes occur over time.
Choosing the right treatment for brain aneurysms is crucial for optimizing outcomes and minimizing risks. Each approach has its unique considerations, and a tailored treatment plan based on individual patient needs is essential for effective management.

Complications and Prognosis
Brain aneurysms present several potential complications that can significantly affect an individual’s health and quality of life. A primary concern associated with aneurysms is the risk of rupture, which can lead to a subarachnoid hemorrhage (SAH). This condition occurs when blood spills into the space between the brain and the innermost layer of membranes covering the brain, leading to severe headaches, nausea, and loss of consciousness. Ruptured aneurysms can have devastating consequences, including brain damage, long-term neurological impairment, or even death. Therefore, early detection and timely management are crucial to mitigate these risks.
Another complication associated with brain aneurysms is the potential for the development of additional aneurysms or vascular malformations. Individuals diagnosed with one aneurysm have a higher predisposition to form others, necessitating ongoing monitoring through medical imaging. Furthermore, untreated brain aneurysms can result in brain ischemia due to impaired blood flow, leading to further neurological issues.
The prognosis for individuals diagnosed with a brain aneurysm varies based on several factors, including the size, location, and whether it has ruptured. Aneurysms that are small and asymptomatic often have a favorable prognosis, and many may not require immediate treatment. This is in stark contrast to larger or symptomatic aneurysms, where surgical intervention could be necessary. Studies suggest that surgical treatments, such as clipping or coiling, significantly improve survival rates and minimize long-term complications. However, the decision on whether to pursue treatment should be tailored to each patient, taking into account the associated risks and benefits.
Ultimately, the management and outcomes of brain aneurysms heavily rely on early diagnosis and appropriate intervention. Ongoing research continues to enhance our understanding of aneurysms, improving prognostic assessments and therapeutic strategies for affected individuals.
Living with a Brain Aneurysm
Receiving a diagnosis of a brain aneurysm can be daunting, but many individuals successfully manage to lead fulfilling lives by making informed lifestyle changes and maintaining close communication with healthcare providers. Recognizing the importance of personalized approaches to health is crucial for those living with this condition.
To begin with, adopting a healthy lifestyle can play a significant role in managing a brain aneurysm. This includes incorporating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, which can help maintain overall health and potentially minimize risks. Regular physical activity is also essential; however, patients should consult with their healthcare team to determine appropriate exercises that will not strain their condition. Additionally, managing stress through mindfulness practices or therapy can be beneficial, as high-stress levels may exacerbate health issues.
An equally important aspect is the adherence to regular follow-ups with healthcare providers. These appointments can help monitor the aneurysm’s size and any changes in the individual’s health status. Medical professionals may recommend imaging tests like MRIs or CT scans periodically to ensure prompt intervention if necessary. Open communication with healthcare providers allows individuals to ask questions, voice concerns, and understand the implications of their condition better.
Support resources are also available for those living with brain aneurysms. Patients and their families can benefit from patient support groups, which provide a platform for sharing experiences, coping strategies, and emotional support. Online forums and local organizations dedicated to brain health can also offer valuable information and connections to mental health professionals who specialize in chronic health conditions.
By implementing these strategies and accessing available resources, individuals diagnosed with a brain aneurysm can lead purposeful lives while managing their health effectively.
Frequently Asked Questions (FAQs)
What is a brain aneurysm?
A brain aneurysm is a bulging or ballooning of a blood vessel in the brain due to a weakness in the vessel wall. It can lead to severe complications if it ruptures, such as a subarachnoid hemorrhage.
What are the symptoms of a brain aneurysm?
Symptoms of an unruptured brain aneurysm may include headaches, vision problems, and pressure behind the eyes. A ruptured aneurysm causes sudden, severe headaches, nausea, vomiting, sensitivity to light, stiff neck, and possibly seizures or loss of consciousness.
What are the main types of brain aneurysms?
The three main types of brain aneurysms are:
- Saccular: The most common, resembling a berry.
- Fusiform: Larger and involving the entire artery.
- Mycotic: Rare, caused by infections.
What causes brain aneurysms?
Genetic conditions, high blood pressure, smoking, and atherosclerosis can increase the risk of developing a brain aneurysm. Family history and other medical conditions like polycystic kidney disease are also contributing factors.
How are brain aneurysms diagnosed?
Brain aneurysms are diagnosed using imaging techniques like CT scans, MRIs, and cerebral angiography. A thorough neurological exam and patient history are also important.
What are the treatment options for brain aneurysms?
Treatments include surgical clipping, endovascular coiling, and flow diversion. The choice of treatment depends on the aneurysm’s size, location, and other individual factors.
What are the risks and complications of brain aneurysms?
The most significant risk is rupture, which can lead to a subarachnoid hemorrhage. Other complications include brain ischemia, the formation of additional aneurysms, and long-term neurological impairment.
What is the prognosis for someone with a brain aneurysm?
The prognosis varies depending on the size, location, and whether the aneurysm has ruptured. Small, unruptured aneurysms may not need immediate treatment, while larger or symptomatic aneurysms require surgical intervention.
Can lifestyle changes help manage a brain aneurysm?
Adopting a healthy lifestyle, including a balanced diet, regular physical activity, and stress management, can help reduce risks. Regular follow-up visits with healthcare providers are essential for monitoring the aneurysm.
Is it possible to live with a brain aneurysm?
Many individuals with brain aneurysms can lead fulfilling lives by making informed decisions about their health and maintaining close communication with healthcare providers. Regular checkups and lifestyle modifications can help manage the condition.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

