Mammary Glands: 7 Shocking Facts You Must Know
Understanding Mammary Glands
Mammary glands are specialized exocrine glands found in mammals, responsible for the production and secretion of milk. These unique structures play a significant role in the reproductive biology of mammals as they facilitate the nourishment of offspring through lactation. The biological significance of mammary glands goes beyond merely providing nutrition; they are also integral to the mother-offspring bonding process, offering immunological protection through colostrum, which is rich in antibodies during the early days of life.
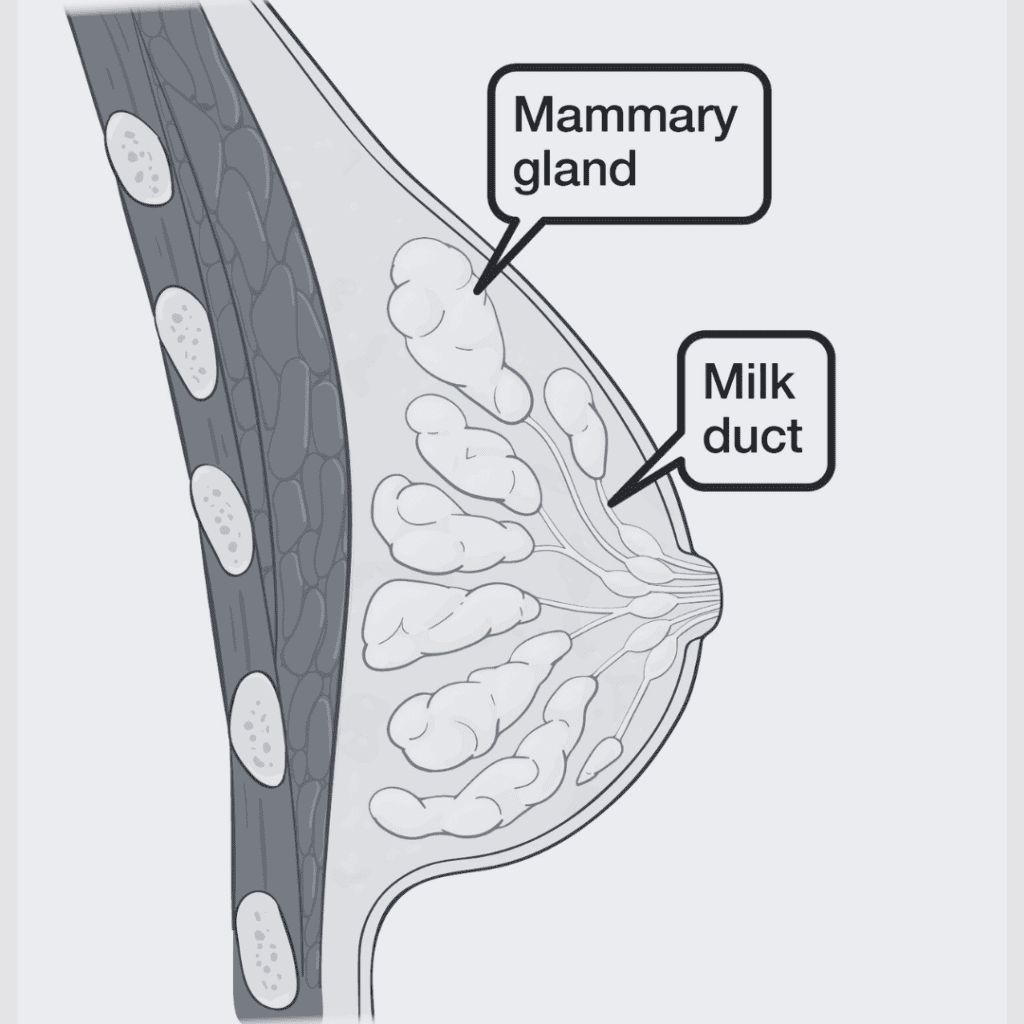
The anatomy of mammary glands is characterized by a complex network of glandular tissue and ducts. In humans, mammary glands are composed of adipose (fat) tissue and glandular tissue, which includes lobules that contain milk-secreting cells called alveoli. Each mammary gland is connected to the nipple via a system of ducts. During lactation, the alveoli contract, pushing the milk into the ducts, which ultimately leads to its expulsion from the nipple during breastfeeding. This anatomical structure reflects the physiological changes that occur during pregnancy and lactation, enabling the production and delivery of milk to the infant.
The regulation of mammary gland function is heavily influenced by hormonal changes, particularly during pregnancy and lactation. Hormones such as prolactin and oxytocin play vital roles in stimulating milk production and ejection, respectively. Understanding these physiological mechanisms is crucial for comprehending various aspects of mammalian reproduction, including the challenges some mothers face related to milk production and breastfeeding. Through the unfolding of these intricate processes and structures within the mammary glands, a clearer picture emerges of their importance in ensuring the survival and health of mammalian offspring.
Anatomy of Mammary Glands
The mammary glands are complex organs essential for lactation in female mammals. Their structure comprises several key components, including lobules, ducts, and supporting tissues, each playing a crucial role in the production and secretion of milk. The foundational units of the mammary glands are the lobules, which consist of clusters of alveoli. These tiny, sac-like structures are lined with specialized epithelial cells responsible for synthesizing milk. Each lobule is surrounded by connective tissue that not only provides structural support but also assists in the overall function of the glands.
Connecting the lobules are the milk ducts, which channel the milk produced in the alveoli toward the nipple. The ducts branch out, forming a network that ensures an efficient transport system for milk during breastfeeding. The terminal duct lobular units (TDLU) represent the most distal regions of the ducts and are typically where milk is gathered before secretion. Hormonal regulation plays a significant role in the growth and function of these components, particularly during pregnancy and lactation, as hormones like prolactin and oxytocin trigger milk production and ejection, respectively.
In addition to lobules and ducts, mammary glands are supported by various tissues, including adipose (fat) tissue and connective tissues. The adipose tissue contributes to the overall size and shape of the breast while also serving as an energy reservoir. Connective tissue, comprised mainly of collagen, helps maintain the integrity and elasticity of the mammary gland structure. The interplay of these anatomical elements forms a well-coordinated system, ensuring the effective production and delivery of milk to nursing offspring. Diagrams illustrating the anatomy of mammary glands can further clarify the relationship between these components and their functional significance in lactation.
Hormonal Regulation of Lactation
The process of lactation, which involves the production and ejection of milk from the mammary glands, is profoundly influenced by several hormones. Among the most significant of these hormones are prolactin and oxytocin, both of which play distinct yet complementary roles in regulating milk production and ejection during breastfeeding. Understanding how these hormones interact is critical for grasping the overall functionality of mammary glands.
Prolactin, secreted by the anterior pituitary gland, is primarily responsible for stimulating milk production. Its levels rise during pregnancy, preparing the mammary glands for lactation. Once childbirth occurs, the reduction in placental hormones triggers a sustained release of prolactin, promoting continuous milk synthesis. The frequency of breastfeeding influences prolactin secretion; the more often a child breastfeeds, the more prolactin is produced, ensuring an adequate milk supply. This positive feedback mechanism is essential for meeting the nutritional needs of the infant.
Oxytocin, on the other hand, is crucial for the ejection of milk from the mammary glands. Released from the posterior pituitary gland, oxytocin is triggered by the mechanical stimulation of the nipples during breastfeeding. This hormone causes the myoepithelial cells surrounding the alveoli in the mammary glands to contract, thereby expelling milk into the ducts and toward the nipple. The interplay between oxytocin and the suckling reflex is vital, as it supports the flow of milk and fosters a bonding experience between mother and child.
Throughout various stages of breastfeeding, the delicate balance of these hormones ensures effective lactation. Factors such as stress, hormonal imbalances, and certain medical conditions can disrupt this regulation, affecting milk production and ejection. Understanding the hormonal basis of lactation equips healthcare professionals with the knowledge to address breastfeeding challenges faced by mothers.

The Process of Milk Production
The biological process of lactogenesis plays a crucial role in the production of milk by mammary glands, which is essential for nourishing infants in their early stages of life. Lactogenesis can be divided into several stages: the first stage, known as colostrogenesis, typically begins during pregnancy, around the second trimester. During this phase, the mammary glands undergo significant changes in preparation for milk production, culminating in the secretion of colostrum. Colostrum is a thick, nutrient-rich fluid produced in the days immediately following birth, containing high levels of antibodies and essential nutrients, making it vital for the infant’s immune system and overall development.
Following colostrum production, the process transitions into the second stage, known as transitional milk production. This phase commences approximately three to five days after delivery and lasts for about two weeks. During this period, the milk composition gradually shifts, with a decrease in protein concentration and an increase in fat content, thus enhancing the caloric density of the milk. This transition is crucial, as the developing infant requires different nutrients at various stages to support their growth and development effectively.
The final stage is characterized by the production of mature milk, which typically occurs around two weeks postpartum. Mature milk is produced in larger quantities and contains a more balanced nutrient composition, designed to meet the ongoing needs of growing infants. The proportion of water, fats, carbohydrates, and proteins in mature milk plays a significant role in the infant’s health and development. This ongoing evolution of milk composition demonstrates the adaptability of mammary glands in response to an infant’s demands, ensuring they receive optimal nutrition for their early growth.
Human Vs. Animal Mammary Glands
The mammary gland serves a crucial role in the sustenance of offspring across various species, providing vital nutrition through milk. While both humans and animals possess mammary glands, there are significant differences in their size, structure, and milk composition, stemming from evolutionary adaptations that enhance survival for both mothers and their young.
Human mammary glands are relatively small compared to those of many other mammals. Typically, human breasts are composed of glandular and adipose tissue, and their size can vary greatly among individuals. Human milk is uniquely formulated for human infants, containing a balance of proteins, fats, and carbohydrates tailored specifically for human development. Notably, human milk contains higher levels of lactose compared to many animal species, facilitating rapid brain development in infants.
In contrast, animal mammary glands exhibit considerable diversity. For instance, the mammary glands of cows and goats are much larger and structured to produce a greater volume of milk. This adaptation is particularly beneficial for species that have multiple offspring or where survival rates depend on the availability of nutrition. The composition of animal milk also varies widely; for example, the milk of some carnivorous species has a higher protein content, aligning with the nutritional needs of their young during growth.
Moreover, evolutionary pressures have influenced the structure of mammary glands. In species such as whales, mammary glands are located internally, allowing for efficient feeding in aquatic environments. This contrast with terrestrial mammals underscores the impressive adaptability of mammary glands to suit the specific needs of different species. Each adaptation serves to ensure that offspring receive optimal nutrition, thereby enhancing their chances for survival and reproductive success.
As we analyze the differences between human and animal mammary glands, it becomes evident that these adaptations are vital for the continuation of species, illustrating the intricate relationship between physiology and survival in the animal kingdom.
Common Disorders of Mammary Glands
Mammary glands, crucial for lactation in females, can be susceptible to a variety of disorders that may impede their function and overall health. Understanding these conditions is important for maintaining breast health and early detection of potential issues. One common disorder is mastitis, which involves inflammation of the mammary glands, often due to bacterial infection. Symptoms typically include redness, swelling, pain in the affected area, and sometimes fever. Women who are breastfeeding are at higher risk for this condition, but it can also occur in non-lactating women and men. Treatment generally involves antibiotics to address the infection and pain management strategies to alleviate discomfort.
Another notable condition is galactorrhea, characterized by the abnormal discharge of milk from the breast not associated with childbirth or nursing. This condition can result from hormonal imbalances, medication side effects, or underlying health issues. Symptoms often include nipple discharge, which may vary in appearance. Women experiencing these symptoms should consult a healthcare provider for an evaluation, as treatment often depends on identifying and addressing the underlying cause.
Breast cancer represents perhaps the most serious disorder affecting mammary glands. Breast cancer may manifest as a lump, changes in breast shape or size, or unusual skin changes. Early detection is key in managing this condition, typically via mammograms and physical examinations. Risk factors may include genetics, age, and lifestyle choices. Treatment options for breast cancer are diverse, ranging from surgery and radiation therapy to chemotherapy and hormone therapy, tailored to the specific type and stage of cancer.
Regular check-ups and breast self-examinations are pivotal in ensuring breast health and facilitating early detection of any abnormalities within the mammary glands. Understanding these common disorders helps in recognizing symptoms promptly and seeking appropriate care. Awareness and education are crucial components in safeguarding breast health.

The Nutritional Value of Milk
Milk, a remarkable fluid produced by mammary glands, serves as an essential dietary staple across various cultures. It is particularly significant in the diets of infants, providing a complete source of nutrition during the early stages of life. The nutritional composition of milk is designed to support growth and development, containing a balanced array of proteins, fats, vitamins, and minerals vital for healthy functioning.
Primarily, milk is rich in high-quality proteins, which are crucial for muscle development and overall bodily repair. Casein and whey proteins—the two main types—offer all the essential amino acids required for human health. The fat present in milk contributes to energy levels and supports the absorption of fat-soluble vitamins (A, D, E, and K). For instance, whole milk contains a significant amount of saturated and unsaturated fats that play important roles in maintaining metabolic functions.
Moreover, milk is a key source of various vitamins and minerals. It is particularly abundant in calcium, which is essential for the development of strong bones and teeth, particularly in children and adolescents. In addition to calcium, milk provides significant amounts of phosphorus, magnesium, and vitamin D, all of which contribute to bone health and metabolic processes. The presence of vitamin B12 in milk is particularly noteworthy as it supports nerve function and the formation of red blood cells.
Additionally, the benefits of milk extend into adult health, contributing to a balanced diet that supports cardiovascular health and weight management, when consumed in moderation. Therefore, the nutritional value of milk produced by mammary glands is multifaceted, making it a crucial component of dietary recommendations and an effective nutritional resource throughout human life stages.
Cultural and Social Aspects of Breastfeeding
Breastfeeding is a practice that is deeply rooted in cultural traditions and societal norms. Across various cultures, perceptions of breastfeeding and the use of breast milk can differ markedly, influencing how mothers are supported and how they approach feeding their infants. In many societies, breastfeeding is not just a biological necessity, but a culturally significant act that fosters bonding between mother and child. For instance, in some Indigenous communities, breastfeeding is viewed as a sacred duty, enriching the practice with spiritual significance. In contrast, in certain urban environments, the emphasis may be more on convenience and personal choice, leading to diverse feeding methods.
Moreover, societal attitudes towards breastfeeding can create significant challenges for new mothers. In environments where public breastfeeding is stigmatized, women may feel pressured to modify their behavior or resort to formula feeding, even if breastfeeding is their preferred option. This societal pressure can eliminate the crucial support that mothers need during the early stages of parenting. Additionally, workplace environments often lack adequate policies to support breastfeeding mothers, such as private lactation rooms and flexible work hours, which can hinder their ability to maintain a breastfeeding routine.
Support systems play a vital role in facilitating successful breastfeeding practices. Community support groups, lactation consultants, and family members can provide the necessary encouragement and guidance for new mothers navigating breastfeeding challenges. These networks are essential, especially in cultures where breastfeeding is less understood or supported. Initiatives promoting awareness about the benefits of breastfeeding can help normalize the practice and encourage societal acceptance. Therefore, fostering a positive and supportive cultural environment will not only aid mothers in their breastfeeding journey but also contribute to healthier generations.
FAQs About Mammary Glands and Lactation
Mammary glands play a vital role in the reproductive biology of mammals, serving as the primary source of nutrition for infants. Despite their importance, misconceptions and concerns about these glands and lactation are prevalent. Below, we address some frequently asked questions to provide clarity and accurate information.
What are mammary glands?
Mammary glands are specialized exocrine glands responsible for the production of milk in female mammals. They develop during pregnancy and undergo significant hormonal changes that prepare them for lactation. The structure of these glands varies among species but generally includes lobules that produce milk, connected to a duct system that delivers milk to the nipple.
How does lactation work?
Lactation is a complex process regulated by hormones such as prolactin and oxytocin. Prolactin stimulates milk production, while oxytocin is responsible for the ejection of milk from the mammary glands. Breastfeeding initiates a feedback loop between mother and infant, with the demand for milk influencing its production. This dynamic ensures that the nutritional needs of the infant are met effectively.
What are common myths about breastfeeding?
Several myths surround breastfeeding, leading to unnecessary anxiety. One common misconception is that nursing mothers cannot engage in any physical activity or exercise, which is untrue. Regular physical activity is generally safe and can even aid in postpartum recovery without hindering milk production. Another myth suggests that maternal diet directly alters the milk’s composition, but while a balanced diet is important for a mother’s health, it minimally impacts the nutritional quality of breast milk.
Is it normal to experience discomfort while breastfeeding?
Discomfort during breastfeeding may occur, especially in the initial days. However, persistent pain is not typical and can indicate issues such as improper latch or mastitis. Consulting a lactation consultant can provide valuable guidance to address these concerns effectively.
By addressing these and other common queries, we hope to enhance understanding of the anatomical and physiological aspects of mammary glands and support informed practices surrounding lactation and breastfeeding.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

