Nomadism: 7 Life-Changing Benefits to Embrace
Understanding Nomadism
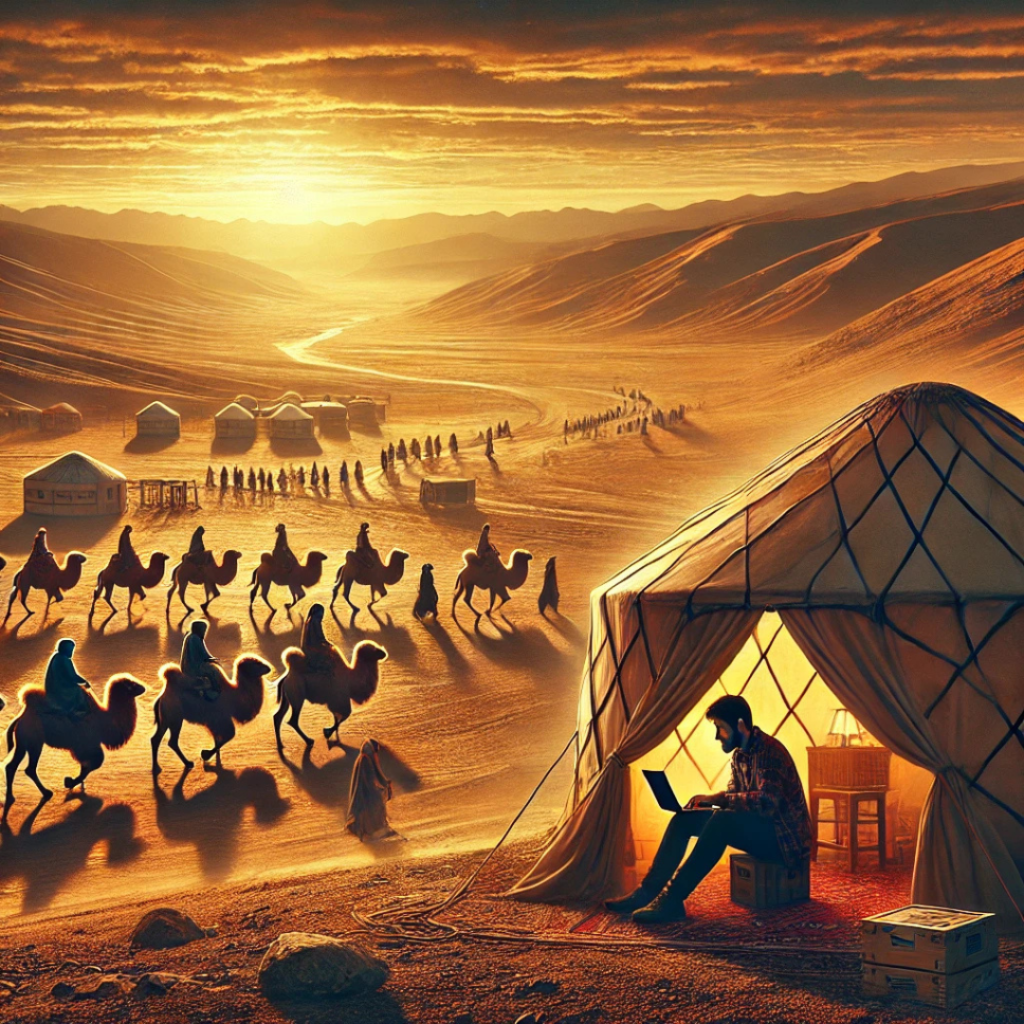
Nomadism refers to a lifestyle characterized by the movement from one place to another, rather than settling permanently in a single location. Historically, nomads have typically engaged in pastoralism, hunting, and gathering, relying on the natural patterns of animal migration and seasonal vegetation growth. This way of life has allowed diverse cultures to flourish across various geographical landscapes, adapting their practices based on the resources available. The significance of nomadic lifestyles throughout history is evident in their influence on trade routes, cultural exchanges, and the spread of knowledge, thereby shaping societies and economies.
Sign up for HUMANITYUAPD
Over time, nomadic lifestyles have undergone substantial transformations. While traditional nomadic practices were often directly tied to survival—such as herding livestock or foraging for food—modern nomadism has evolved into a more complex phenomenon. Today, the concept includes a broad spectrum of practices, from digital nomadism, where individuals work remotely while traveling, to lifestyle nomadism, where people seek varied experiences across different cultures. This evolution reflects broader societal changes, including advances in technology, communication, and transportation, enabling mobility in ways that were previously unthinkable.
Understanding nomadism is increasingly relevant in contemporary society. The rise of remote work and the gig economy has led many individuals to adopt a nomadic lifestyle by choice rather than necessity. The growing interconnection among global populations fosters cross-cultural interactions that enrich societal perspectives and dialogues. Moreover, economic implications of nomadism can also be observed in tourism and the sharing economy, where nomadic lifestyles contribute significantly to local economies. Awareness of nomadic practices thus provides insight into cultural adaptability, resilience, and the social fabric of our interconnected world.
➡️ Table of Contents ⬇️
Types of Nomadic Societies
Nomadic societies can be broadly categorized into several distinct types, each exhibiting unique lifestyles, cultures, and adaptations to their environments. The primary categories include pastoral nomads, hunter-gatherers, and more contemporary forms of nomadism, such as digital nomads. Each of these groups contributes to our understanding of nomadic lifestyles in diverse ways.
Pastoral nomads primarily rely on the herding of livestock for their subsistence. This way of life involves migrating seasonally with their animals to access fresh pastures and water sources. Common in regions such as Central Asia and the Arabian Peninsula, pastoral nomads maintain complex social structures defined by kinship ties and shared responsibilities among community members. They often engage in trade with settled agricultural societies, exchanging animal products for grains and other necessities.
Hunter-gatherers represent one of the earliest forms of human lifestyle. These nomadic groups move continuously in search of wild plants and animals, reflecting an adaptive strategy to their natural surroundings. With societies ranging from the Indigenous peoples of the Arctic to the San people of Southern Africa, hunter-gatherers exhibit a deep knowledge of their ecosystems. Their social structures tend to be egalitarian, often with decisions made collectively. The mobility of hunter-gatherers allows them to efficiently exploit seasonal resources, ensuring survival and cultural continuity.
Modern digital nomads have redefined traditional notions of nomadism by leveraging technology to work remotely while traveling. This type of nomadism has surged with advancements in communication technology, enabling individuals to maintain careers in various fields while living in diverse locations around the globe. Common among millennials, digital nomads often adopt a lifestyle that prioritizes flexibility and personal experiences over physical permanence, significantly impacting local economies and tourism sectors.
In conclusion, the rich tapestry of nomadic societies reveals a spectrum of adaptations and interactions with different environments. Understanding these groups not only illuminates their unique cultures and economies but also highlights the resilience and innovation inherent in the nomadic way of life.
The Economics of Nomadism
Understanding the economics of nomadism reveals a complex interplay between mobility and resource management. Nomadic lifestyles are sustained through various means, including trade, livestock management, and foraging. Each of these activities not only provides the necessities for survival but also contributes to the local and, in some cases, global economies. For many nomadic groups, livestock, particularly, plays a pivotal role in their economic framework. Herding practices allow nomads to utilize vast territories, enriching their diets with milk, meat, and hides while also serving as a wealth indicator within their communities.
Trade is another critical economic aspect. Nomads often engage in barter with sedentary communities, exchanging animal products for grains, tools, and textiles. This symbiotic relationship enhances both parties’ economic viability; nomads gain access to resources otherwise unavailable in their mobile lifestyle, while sedentary communities benefit from high-quality animal products. Additionally, nomadic groups are increasingly participating in broader economic activities, such as tourism, where cultural exchange can foster sustainable incomes. In this regard, the unique traditions and knowledge of nomadic peoples become valuable commodities in the global marketplace.
The relationship between resource management and mobility is crucial; nomads often practice sustainable land-use techniques that ensure minimal impact on the ecosystems they traverse. Their traditional ecological know-how allows them to manage pastures and other resources responsibly, thus promoting biodiversity. In contrast, modern agricultural practices often lead to degradation and depletion of resources. Learning from nomadic practices can inform contemporary economic systems, advocating for sustainable practices that align with environmental preservation.
In essence, the economics of nomadism highlight an intricate balance of trade, resource management, and cultural exchange. As the world increasingly grapples with sustainability issues, the insights gained from nomadic lifestyles can play a vital role in creating more resilient and adaptable economic systems.

Cultural Practices and Traditions
Nomadic lifestyles, characterized by their mobility and adaptability, are deeply intertwined with the cultural practices and traditions of the communities that practice them. These cultures are not static; they evolve in response to their environment and the changes they encounter. One of the most significant aspects of nomadic cultures is their unique customs, which may include rituals and practices handed down through generations. These customs often reflect the solidarity within the community and the relationships they maintain with the land and each other.
Language serves as a vital tool for the expression and preservation of cultural identity among nomadic groups. Many communities possess distinct dialects or languages that are rich in oral literature, encompassing stories, proverbs, and songs that outline their history, values, and experiences. These narratives are essential for passing down knowledge and traditions, fostering a sense of belonging while enhancing their cultural identity.
Art forms play an integral role in nomadic cultures, often serving practical purposes while being aesthetically significant. Handicrafts, textiles, and traditional music encapsulate the values and beliefs of these communities, offering a glimpse into their way of life. Artists within these groups not only create for survival but also convey their histories and worldviews through their work, celebrating their rich heritages.
Storytelling, rituals, and community celebrations are pivotal in reinforcing social bonds and preserving the heritage of nomadic societies. These activities are often anchored in significant life events, seasonal changes, or communal accomplishments. They serve not only as means for entertainment but also as vital mechanisms for social cohesion and mutual support. Through gatherings, individuals share experiences and maintain their cultural legacies, ensuring that future generations continue to recognize the importance of their unique lifestyles.
Challenges Faced by Nomads Today
The modern landscape presents a myriad of challenges for nomadic communities that have historically thrived through their mobility and adaptability. One significant issue is climate change, which directly impacts their traditional grazing routes and seasonal migrations. Altered weather patterns can lead to droughts or unpredictable rainfall, affecting the availability of natural resources essential for their livestock. As these environmental changes escalate, nomads are often forced to abandon their ancestral lands in search of more sustainable living conditions.
Land rights issues further complicate the situation for many nomadic populations. Governments around the world increasingly prioritize territorial claims and land use policies that disregard the customary practices of nomadic lifestyles. This results in restricted access to vital grazing areas and essential water sources, limiting their ability to sustain their herds and, consequently, their livelihoods. In many cases, laws that favor agricultural or urban development marginalize nomads, pushing them toward undesirable living conditions and eroding their cultural identities.
Globalization has also brought profound shifts to the nomadic way of life. While it has opened up new opportunities for economic exchange, it often undermines traditional practices. Increasing commercial pressures can result in the commodification of nomadic culture, where the authenticity of their lifestyle is sacrificed for tourism or marketability. Furthermore, urbanization inflates the migration towards cities, causing younger generations to abandon nomadic practices for settled lives with perceived greater security and opportunity. This shift can lead to the gradual dissolution of distinct cultural identities that have been cultivated over generations.
Thus, nomads today navigate a complex interplay of environmental, social, and political challenges that threaten their traditional practices and way of life. Addressing these issues requires a holistic approach that considers the rights and needs of nomadic communities within contemporary policy frameworks. Only then can we foster an understanding and appreciation of the invaluable contributions that these mobile societies offer to our world’s cultural tapestry.
The Role of Technology in Modern Nomadism
The advent of technology has significantly transformed the landscape of modern nomadism, making it increasingly feasible for individuals to live a transient lifestyle while maintaining professional obligations. Digital nomads, in particular, benefit from a range of technological tools that facilitate remote work, streamline travel planning, and enhance communication. Applications like Zoom and Slack have revolutionized the way digital nomads interact with colleagues and clients, allowing for seamless collaboration regardless of geographical boundaries.
Moreover, cloud-based platforms such as Google Drive and Dropbox offer secure and easily accessible storage solutions for nomads who require their documents on-the-go. This accessibility not only enhances productivity but also provides a sense of stability amidst the often unpredictable nature of a nomadic lifestyle. The ability to work from various locations has resulted in a significant increase in opportunities for professionals across multiple disciplines, enabling them to balance work and travel in unprecedented ways.
However, the reliance on technology also carries challenges. While it fosters connectivity in many areas, it can also contribute to feelings of isolation and disconnection from traditional practices. Nomads may find themselves physically alone in a new environment, leading to a paradox where increased digital communication ironically diminishes face-to-face interactions. Furthermore, technological over-dependence can detract from immersing oneself in local cultures, as the focus shifts from genuine experiences to maintaining a digital presence.
In this context, it is essential for modern nomads to strike a balance between leveraging technology for their professional needs while also engaging meaningfully with the surrounding communities. As modern nomadism continues to evolve, understanding technology’s multifaceted role will be crucial for individuals navigating this dynamic lifestyle.

Comparative Analysis: Nomadic vs. Sedentary Lifestyles
Nomadic and sedentary lifestyles represent two distinct ways of living, each with its own set of advantages and challenges. Understanding these differences can shed light on the impact of these lifestyles on individuals and societies. While both approaches to living have valid points, examining their implications regarding environmental sustainability, economic practices, cultural richness, and social dynamics can provide valuable insights.
Nomadic lifestyles, characterized by constant movement and adaptability to various environments, often showcase a harmonious relationship with nature. Nomads typically engage in sustainable practices, utilizing resources in a way that minimizes environmental degradation. For instance, many nomadic groups rotate grazing areas for livestock to avoid overgrazing and maintain ecosystem balance. On the contrary, sedentary lifestyles can lead to significant environmental impacts, particularly through urbanization and industrialization, which can result in habitat destruction and pollution.
From an economic standpoint, nomadic communities often rely on diverse income sources, drawing from local environments. This economic flexibility can serve as an advantage in fluctuating market conditions. However, the reliance on traditional practices may also limit access to modern economic opportunities. On the other hand, sedentary populations benefit from stable economies and employment opportunities in urban areas, but they may face challenges related to economic volatility and disparities in resource distribution.
Culturally, nomadic lifestyles often foster rich traditions and social networks that emphasize community and resilience. The sharing of skills and stories contributes to a dynamic cultural tapestry that can inspire future generations. In contrast, sedentary lifestyles tend to promote cultural assimilation and the homogenization of practices due to urban influences. Yet, cities can also be cultural hubs, fostering diversity and innovation.
When analyzing social dynamics, nomadic groups may exhibit strong social bonds tied to shared experiences and mutual dependence. Conversely, sedentary lifestyles can encourage both community cohesion and social isolation, as urban environments may create barriers for connection among individuals.
In today’s interconnected world, recognizing the value of both nomadic and sedentary lifestyles is crucial. Balancing their strengths and weaknesses may lead to more sustainable and enriching ways of living, promoting respect for diverse cultural practices and environmental stewardship.
Future of Nomadism
The future of nomadism is poised to undergo significant transformations as global landscapes evolve due to various socio-economic and environmental factors. One evident trend is the resurgence of interest in nomadic living, particularly among younger generations. This demographic appears increasingly attracted to alternative lifestyles that prioritize flexibility, sustainability, and experiential learning over conventional stability. With advancements in technology, particularly in remote work capabilities, individuals now have the opportunity to engage in nomadic lives without sacrificing professional aspirations. This shift in work culture has inadvertently normalized the practice of living on the move.
Climate change presents a complex backdrop that will likely influence nomadic patterns in the coming years. As certain regions become less hospitable due to rising temperatures, droughts, or natural disasters, communities may be forced to adopt more fluid settlement strategies. This mobility could lead to the evolution of contemporary nomadic practices, where individuals and groups migrate in response to environmental challenges. The implications for cultural survival are profound, as traditional knowledge and lifestyles may be vital for adapting to changing ecosystems. Sustainable nomadic practices might emerge, where communities contribute to ecological preservation while maintaining their unique cultural identities.
Integrating nomadic practices into broader societal frameworks can yield multiple benefits, such as enhanced cultural exchange, innovative problem-solving, and increased resilience against environmental changes. Urban areas may adapt to support transient populations, mirroring the characteristics of traditional nomadic societies. This integration may foster a greater appreciation for the values of mobility and adaptability within static communities, ultimately contributing to a enriched societal tapestry. As we look ahead, the dialogue surrounding nomadism will be essential to create inclusive environments that recognize the contributions and challenges of nomadic lifestyles while promoting the sustainability of these practices amid a rapidly changing world.
Frequently Asked Questions (FAQs) About Nomads
Nomadic lifestyles, characterized by constant movement and adaptability, often lead to various inquiries regarding practical aspects of life in transit. Here, we address some of the most common questions related to health care, education, legal status, and social integration faced by nomads.
What about healthcare for nomads?
Accessing healthcare can be challenging for those leading a nomadic lifestyle, yet many countries provide temporary health insurance options. Nomads often rely on international health insurance that covers medical emergencies worldwide. Consulting local healthcare providers in each destination and utilizing telemedicine services can also help ensure proper health management while on the road.
How do nomads manage their education?
Education for children of nomadic families can be facilitated through a variety of approaches, including online schooling, distance learning programs, and community-based educational initiatives. Many nomadic parents opt for homeschooling, allowing flexibility in their schedule while ensuring that educational needs are met. Various organizations also provide resources catered to nomadic families, addressing specific educational challenges.
What is the legal status of nomads?
Legal recognition varies significantly by country. Nomads may face unique legal challenges regarding visas and residency permits. Some nations offer special visas for digital nomads, promoting the legal right to live and work remotely. However, it is crucial for individuals to research and comply with local laws to avoid potential legal issues during their travels.
How do nomads integrate with the broader society?
Integration into local communities can vary widely among nomads. Many actively participate in local cultural events, volunteer opportunities, and social networks to foster connections. Building relationships with local residents can lead to a deeper understanding of the culture and create a sense of belonging, even if only temporarily in the area.
By addressing these frequently asked questions, we can shed light on the intricacies and realities of nomadic lifestyles, helping to clarify misconceptions while providing valuable insights.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

