Pelvis (Pelvic) Strength: 6 Essential Movements
Understanding the Pelvis
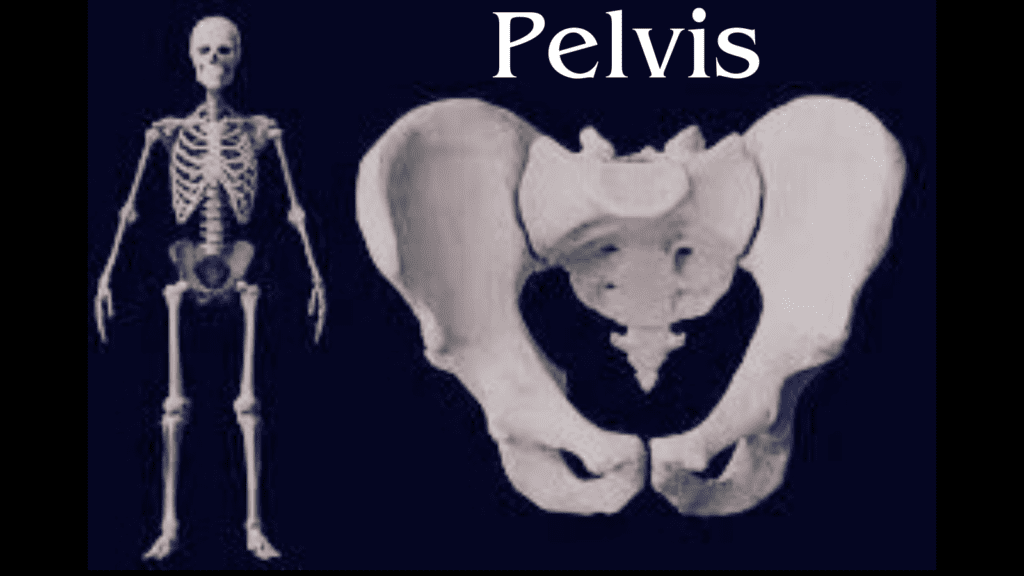
The pelvis is a complex and vital structure in human anatomy, serving as a crucial component in the skeletal system. Situated at the base of the spine, the pelvis connects the axial skeleton to the lower limbs, thereby playing a significant role in mobility and stability. Its composition includes various bones such as the ilium, ischium, and pubis, which form a bony ring that encases and protects the pelvic organs. Additionally, the sacrum and coccyx contribute to the overall structure, making the pelvis a pivotal point for both support and movement.
The significance of the pelvis extends beyond mere support of the skeleton; it is integral to multiple bodily functions. For instance, it plays a critical role in locomotion, serving as an anchor point for muscles that facilitate walking and running. Furthermore, the pelvis supports and contains vital organs, including the bladder, reproductive organs, and parts of the digestive system, thus contributing to their functional efficiency. The design of the pelvis also aids in childbirth, as its shape and flexibility accommodate the passage of the newborn during delivery.
In addition to its anatomical importance, the pelvis has implications for overall health and fitness. Abnormalities or injuries in the pelvic region may lead to a wide range of complications, including pain, reduced mobility, or dysfunction of the organs it supports. Therefore, understanding the anatomy and function of the pelvis is essential for both medical professionals and individuals seeking to maintain their health. This introduction sets the stage for a deeper exploration of the pelvis, its anatomy, and its health implications in the sections that follow.
Anatomy of the Pelvis
The pelvis is a complex anatomical structure that plays a crucial role in the human body. It is primarily composed of several bones, including the ilium, ischium, pubis, sacrum, and coccyx. These bones form a bowl-like shape, supporting the weight of the upper body when sitting and standing, and they provide attachment points for a variety of muscles and ligaments that are essential for movement and stability.
The pelvic region can be subdivided into two main parts: the false pelvis and the true pelvis. The false pelvis, or greater pelvis, is the upper portion that helps support abdominal organs, while the true pelvis, or lesser pelvis, contains the pelvic cavity and is significant for reproductive and excretory functions. The pelvic inlet, an important boundary located at the top of the true pelvis, comprises the pubic symphysis, sacral promontory, and the arcuate line of the ilium. On the other hand, the pelvic outlet is formed by the ischial tuberosities, pubic arch, and the tip of the coccyx, providing a regulated passage for childbirth.
It is essential to note the anatomical distinctions between male and female pelvises. Generally, the female pelvis is broader and has a larger pelvic inlet and outlet, adapting for childbirth. In contrast, the male pelvis is typically narrower and more rugged, optimized for bipedal locomotion and structural stability. These differences not only influence reproductive health but also affect overall biomechanics and movement patterns in individuals.
Understanding the anatomy of the pelvis is vital for recognizing its function in supporting the body and facilitating essential activities. Awareness of the pelvic structure can lead to better health practices and informed medical interventions related to pelvic disorders.
Functions of the Pelvis
The pelvis serves multiple crucial functions that are essential for human anatomy and overall health. Primarily, it plays a significant role in locomotion, acting as a primary anchor point for the lower limbs and providing stability during movement. The greater pelvis, or pelvis major, supports the abdominal organs, while the lesser pelvis, or pelvis minor, is essential for the support of reproductive organs. This structural arrangement facilitates a wide range of motions, allowing for walking, running, and jumping. The pelvic girdle acts as a shock absorber during these activities, which is vital for protecting the spine and other structures.
Another critical function of the pelvis is its involvement in childbirth. The female pelvis is specifically adapted to accommodate the birthing process, offering a wider canal for the passage of the baby. The shape and dimensions of the pelvic inlet and outlet can significantly influence labor and delivery outcomes. Additionally, hormonal changes during pregnancy can affect the pelvis, enabling it to become more flexible as labor approaches. This adaptability is essential for minimizing the risks involved in childbirth, making an understanding of pelvic anatomy crucial for obstetric care.
The pelvis also acts as a support structure for the spine and internal organs. It provides a strong foundation for the vertebral column, allowing for an efficient transfer of weight from the upper body to the lower limbs. The pelvic floor muscles, which span the space beneath the pelvis, play a vital role in supporting the bladder, rectum, and uterus, contributing to the maintenance of bodily functions. Weakness or dysfunction in these muscles can lead to issues such as incontinence or pelvic organ prolapse, emphasizing the importance of pelvic health. Overall, the pelvis is integral to locomotion, childbirth, and the overall support of critical structures in the body.

Common Pelvic Disorders
The pelvis is a crucial component of the human anatomy, and various disorders can affect this region, leading to significant discomfort and health concerns. Among these, pelvic pain, pelvic organ prolapse, and pelvic inflammatory disease are particularly prevalent. Understanding these conditions along with their symptoms and risk factors is essential for effective management and treatment.
Pelvic pain is often characterized as a persistent discomfort occurring in the lower abdomen or pelvis. It can arise from numerous sources, such as reproductive issues, gastrointestinal disturbances, or urinary problems. Recent studies indicate that chronic pelvic pain affects about 15% of women worldwide, with factors such as endometriosis, irritable bowel syndrome, and even muscle tension contributing to the perception of pain. Symptoms may vary significantly, encompassing sharp or dull aching sensations, and might be exacerbated during menstruation, intercourse, or physical activity.
Another notable condition is pelvic organ prolapse, which occurs when the pelvic organs, such as the bladder, uterus, or rectum, descend into the vaginal canal due to weakened pelvic muscles or connective tissues. This disorder is more common in women who have given birth, particularly vaginally, and those who have undergone menopause. Risk factors include advancing age, obesity, and a history of pelvic surgery. Common symptoms of pelvic organ prolapse include feelings of heaviness in the pelvic area, urinary incontinence, and discomfort during intercourse.
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs, often stemming from sexually transmitted infections. PID can result in severe complications, including infertility, chronic pelvic pain, and ectopic pregnancy. It predominantly affects sexually active women under the age of 25, with risk factors including multiple sexual partners and a history of STIs. Signs of PID range from mild to severe and may include lower abdominal pain, fever, unusual vaginal discharge, and pain during intercourse.
Pelvic Floor Muscles: Importance and Exercises
The pelvic floor muscles play a significant role in the overall health and function of the pelvic region. This group of muscles forms a supportive hammock across the pelvic cavity, stabilizing the pelvic organs such as the bladder, intestines, and uterus. A strong and well-functioning pelvic floor is crucial for maintaining optimal urinary and bowel control, sexual function, and support for the lumbar spine. Weak pelvic floor muscles can lead to a range of concerns, including incontinence, pelvic organ prolapse, and decreased sexual satisfaction.
Incorporating exercises specifically targeted at strengthening the pelvic floor can enhance muscle tone and function. One of the most commonly recommended exercises is the Kegel exercise, which involves repeatedly contracting and relaxing the pelvic floor muscles. To perform Kegel exercises, one should first identify the pelvic floor muscles by attempting to stop urination mid-stream. Once recognized, the individual can practice contracting the muscles for a count of three, followed by a relaxation phase of the same duration. This cycle can be repeated several times, aiming for three sets of 10 repetitions daily.
In addition to Kegels, other exercises, such as bridges and squats, can also promote pelvic floor strength effectively. These movements engage not only the pelvic muscles but also the glutes and core, contributing to overall stability and strength. Similarly, yoga and pilates routines often include poses that target the pelvis, fostering both flexibility and strength within the region.
Maintaining a strong pelvic floor has numerous benefits, including improved bladder control, enhanced sexual health, and decreased risk of pelvic organ prolapse. Regular practice of targeted exercises contributes significantly to pelvic health, making it paramount for individuals to incorporate these movements into their daily routines. Ultimately, strengthening pelvic floor muscles is crucial for maintaining overall well-being and functional capability.
Impact of Lifestyle on Pelvic Health
The health of the pelvic region is significantly influenced by various lifestyle factors, including diet, physical activity, and posture. Understanding these impacts can empower individuals to make informed decisions that contribute to optimal pelvic health. A balanced diet plays a crucial role in maintaining pelvic function. Consuming a variety of nutrients, particularly those rich in fiber, can promote regular bowel movements and prevent constipation, a condition that may lead to pelvic floor stress. Incorporating foods high in antioxidants and anti-inflammatory compounds, such as fruits, vegetables, and whole grains, can also support overall muscle and tissue health in the pelvic area.
Physical activity is another critical factor that affects pelvic health. Engaging in regular exercise strengthens the pelvic floor muscles and enhances overall body awareness. Activities such as yoga and Pilates focus on core strength and flexibility, providing an effective means to maintain pelvic stability. Furthermore, cardiovascular exercises such as walking, swimming, or cycling can enhance blood flow to the pelvic region, promoting its health. It is essential to balance high-impact activities with low-impact options to avoid excessive strain on the pelvic muscles.
Posture should not be overlooked when considering pelvic health. Poor posture, especially during sitting, can lead to undue pressure on the pelvic organs and muscles. Maintaining an aligned and neutral spine while sitting, standing, or bending can mitigate such risks. Ergonomic furniture and proper sitting techniques should be adopted, particularly for individuals who spend long hours at desks. Additionally, mindfulness regarding how to lift heavy objects safely can also help in preventing pelvic issues.
Incorporating these lifestyle adjustments into daily routines can significantly enhance pelvic health. Making conscious choices regarding diet, engaging in regular exercise, and practicing good posture are fundamental steps toward ensuring the well-being of the pelvic region.

Preventive Measures for Pelvic Health
Maintaining pelvic health is essential for overall well-being. To ensure the proper functioning of the pelvic region, a series of preventive measures can be adopted. One of the most significant steps is to schedule regular check-ups with a healthcare professional. These consultations offer opportunities to identify any abnormalities or potential issues early on, facilitating timely interventions. Routine screenings can also empower patients with knowledge regarding their pelvic health, fostering a proactive approach to wellness.
Moreover, becoming aware of the symptoms that may indicate pelvic disorders is crucial. Symptoms such as pelvic pain, urinary changes, or unusual bleeding should never be overlooked. Recognizing these warning signs early can lead to appropriate medical consultations and interventions that may stave off more severe complications. Patients are encouraged to engage in open dialogues with healthcare providers about their concerns, thereby nurturing a collaborative relationship geared towards maintaining pelvic health.
In addition to regular screenings and symptom awareness, an active lifestyle significantly contributes to pelvic health. Engaging in regular physical activity, especially exercises that strengthen the pelvic floor, can help maintain function and prevent issues such as incontinence and pelvic organ prolapse. Low-impact exercises, such as walking, swimming, or yoga, are excellent options. Furthermore, women are encouraged to explore pelvic floor exercises, also known as Kegel exercises, which can be beneficial in enhancing muscle strength and resilience.
In essence, a holistic approach encompassing regular health check-ups, awareness of symptoms, and an active lifestyle will bolster pelvic health. Taking proactive measures can lead to better outcomes and enhance the quality of life, making it imperative for individuals to prioritize their pelvic health.
Research and Advances in Pelvic Health
Recent years have seen significant advancements in the field of pelvic health, driven by ongoing research and technological innovations. Pelvic disorders, which encompass a range of conditions affecting the pelvic region, have garnered increased attention from medical professionals and researchers alike. With this focus, new treatment options are emerging that aim to improve patient outcomes and overall quality of life.
One notable advancement in pelvic health is the development of minimally invasive surgical techniques. These procedures often result in reduced recovery times and less postoperative pain compared to traditional surgery. For instance, laparoscopic and robotic-assisted surgeries have become increasingly popular for treating various pelvic conditions, such as uterine fibroids and endometriosis. These innovations allow for precise interventions with fewer complications, which can significantly enhance the patient’s experience and recovery process.
Technological innovations in diagnostic methods also play a crucial role in advancing pelvic health. Imaging techniques, such as high-resolution ultrasound and magnetic resonance imaging (MRI), have improved the accuracy of diagnoses for pelvic disorders. These advances enable healthcare providers to identify issues at earlier stages, leading to more effective management strategies. Additionally, the adoption of telemedicine has made it easier for patients to access specialists and receive follow-up care, especially in remote areas.
Furthermore, ongoing research focuses on understanding the underlying causes of pelvic disorders, including hormonal, genetic, and lifestyle factors. Recent studies have shed light on the interplay between pelvic health and other bodily systems, emphasizing the importance of a holistic approach to treatment. As our understanding of these complex relationships grows, healthcare providers can develop more tailored interventions, ensuring better management of pelvic conditions.
In conclusion, the field of pelvic health is continually evolving, driven by innovative treatments, advanced diagnostic technologies, and a deeper understanding of the factors impacting pelvic disorders. Staying abreast of these developments is crucial for both healthcare providers and patients as they navigate the management of pelvic health issues.
Frequently Asked Questions (FAQs)
What is the function of the pelvis?
The pelvis serves multiple key functions, which include supporting the weight of the upper body while sitting and standing, facilitating movement through its connection to the femur (thigh bone), and housing vital organs in the reproductive and urinary systems. Furthermore, the pelvis plays a crucial role during childbirth, enabling the passage of the baby through the birth canal.
What are common disorders of the pelvis?
A number of disorders can affect the pelvis, including pelvic inflammatory disease, pelvic floor dysfunction, and hernias. Musculoskeletal issues such as sacroiliac joint dysfunction or hip osteoarthritis can also contribute to pelvic pain. Understanding these conditions is essential for effective diagnosis and treatment, as they can significantly impact an individual’s quality of life.
How can I maintain a healthy pelvis?
Maintaining a healthy pelvis often requires a multi-faceted approach. Regular exercise focusing on pelvic floor muscle strengthening, flexibility training, and overall fitness can help maintain proper pelvic alignment and function. Additionally, practicing good posture and ergonomics can alleviate strain on the pelvic region. It is advisable to incorporate stretching exercises, such as yoga, to promote flexibility and reduce tension. Dietary choices play a role as well; a balanced diet rich in nutrients supports overall health, including the pelvic area.
When should I seek medical advice for pelvic issues?
Individuals should consider consulting a healthcare professional if they experience chronic pain, discomfort, or any other unusual symptoms in the pelvic region. Signs such as significant pain during menstruation, sexual intercourse, or sudden changes in urinary or bowel habits should prompt an evaluation. Early diagnosis of pelvic disorders can lead to more effective management and improved health outcomes.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

