Understanding Sleep Apnea
Sleep apnea is a common but often under diagnosed sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions, known as apneas, can last from a few seconds to minutes and may occur multiple times throughout the night. In some cases, periods of shallow breathing, referred to as hypopneas, also disrupt the sleep cycle. The condition can significantly affect the quality of sleep, leading to daytime fatigue, irritability, and other health complications.
Understanding sleep apnea is crucial given its widespread prevalence and potential impact on overall health. It is estimated that millions of individuals globally suffer from this condition, with many remaining undiagnosed. Sleep apnea is more common in individuals who are overweight, older adults, and men, although it can affect anyone, including children. The disorder is associated with serious health risks such as cardiovascular disease, hypertension, diabetes, and stroke. Moreover, untreated sleep apnea can impair cognitive function, reduce productivity, and increase the risk of motor vehicle accidents due to excessive daytime sleepiness.
Given these significant implications, raising awareness about sleep apnea is essential. Public education and early diagnosis can help mitigate the adverse health effects and improve the quality of life for those affected. In subsequent sections, this blog will delve deeper into the causes, symptoms, and available treatments for sleep apnea. By comprehensively understanding this condition, individuals can take proactive steps towards effective management and better health outcomes.
Sleep apnea is a disorder characterized by interruptions in breathing during sleep. These interruptions, known as apneas, can have significant health impacts if left untreated. There are three primary types of sleep apnea: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (also known as treatment-emergent central sleep apnea). Understanding the distinctions between these types is critical for effective diagnosis and treatment.
- Obstructive Sleep Apnea (OSA)
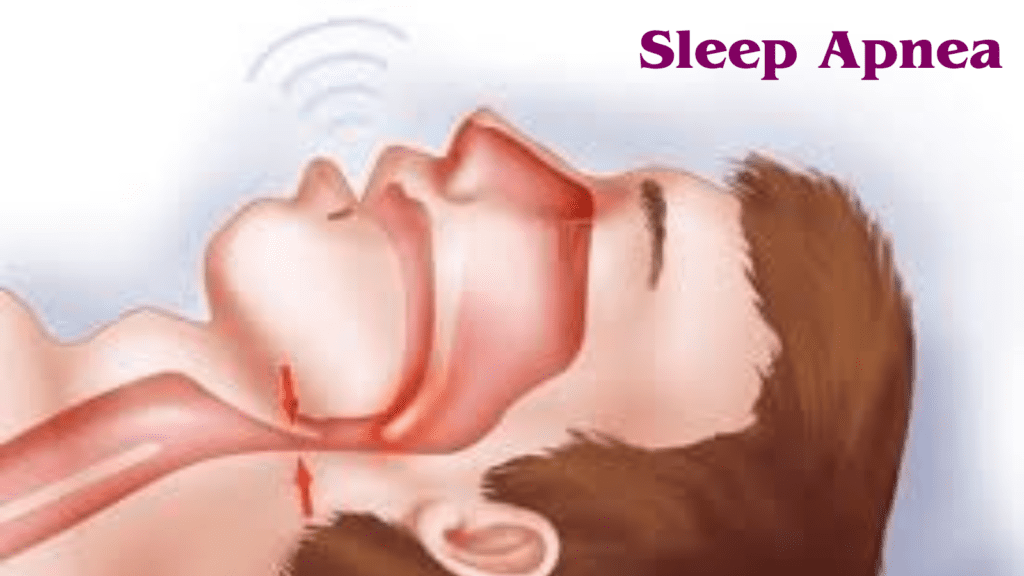
Obstructive sleep apnea (OSA) is the most common form of sleep apnea. It occurs when the muscles in the throat relax excessively during sleep, causing a temporary obstruction of the airway. This blockage results in reduced or completely halted airflow, leading to repeated awakenings throughout the night as the body struggles to reopen the airway. Common causes of OSA include obesity, anatomical abnormalities, and genetic predispositions. The condition is often characterized by loud snoring, gasping, or choking sounds during sleep. Individuals with OSA may experience excessive daytime sleepiness, cognitive impairments, and an increased risk of cardiovascular diseases.
- Central Sleep Apnea (CSA)
Central sleep apnea (CSA) is less common than OSA and involves a different mechanism. In CSA, the brain fails to send appropriate signals to the muscles responsible for controlling breathing. This lack of communication results in periods where the individual makes no effort to breathe, leading to disrupted sleep and decreased oxygen levels. CSA can be associated with certain medical conditions such as heart failure, stroke, or the use of specific medications. Unlike OSA, CSA typically does not involve physical airway obstruction, and snoring is less prevalent. Symptoms may include frequent awakenings, insomnia, and daytime fatigue.
- Complex Sleep Apnea Syndrome
Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, is a combination of both OSA and CSA. This type of sleep apnea is identified when individuals with obstructive sleep apnea develop central apneas after receiving continuous positive airway pressure (CPAP) therapy, which is a common treatment for OSA. The exact cause of complex sleep apnea syndrome remains unclear, but it is thought to involve a mix of obstructive and central mechanisms. This condition can be particularly challenging to treat and often requires a tailored therapeutic approach to address both components effectively.
Causes and Risk Factors
Sleep apnea is a multifaceted condition influenced by a variety of causes and risk factors. Genetic predisposition plays a significant role, with studies indicating that individuals with a family history of sleep apnea are more likely to develop the condition. This genetic link can result in inherited anatomical characteristics, such as a narrow airway, that predispose someone to sleep apnea.
Lifestyle choices are also pivotal in the onset of sleep apnea. Obesity is a primary risk factor; excess weight, particularly around the neck, can obstruct the airway. Additionally, the consumption of alcohol and sedatives can relax the muscles of the throat, exacerbating airway blockage during sleep. Smoking is another contributing factor, as it can cause inflammation and fluid retention in the upper airway, further narrowing the passage.
Several underlying health conditions are associated with an increased risk of sleep apnea. Conditions such as hypertension, type 2 diabetes, and cardiovascular diseases are commonly linked with sleep apnea. These health issues can create a vicious cycle, where sleep apnea exacerbates the condition, which in turn worsens the sleep apnea.
Demographic factors also influence the likelihood of developing sleep apnea. Age is a significant factor, with the prevalence of sleep apnea increasing as people age, particularly after the age of 40. Gender differences are notable as well; men are more likely to develop sleep apnea than women, although the risk for women increases after menopause. Anatomical differences such as a deviated septum, enlarged tonsils, or a large tongue can also contribute to airway obstruction, increasing the risk of sleep apnea.
Understanding these causes and risk factors is crucial for both prevention and management of sleep apnea. Recognizing the multifaceted nature of this condition allows for a comprehensive approach to treatment and lifestyle adjustments, ultimately improving quality of life for those affected.

Symptoms and Warning Signs
Sleep apnea is a serious sleep disorder characterized by repeated interruptions in breathing during sleep. Recognizing the symptoms and warning signs of sleep apnea is crucial for timely diagnosis and treatment. These symptoms can manifest both during the night and throughout the day, significantly impacting an individual’s overall health and well-being.
Nighttime symptoms of sleep apnea are often the most noticeable and include loud snoring, gasping for air, and frequent awakenings. Loud snoring is typically one of the earliest and most common indicators. This snoring is often punctuated by periods of silence followed by gasping or choking sounds, signifying a temporary cessation of breathing. These interruptions can cause the person to wake up multiple times during the night, leading to fragmented and non-restorative sleep.
During the day, individuals with sleep apnea may experience excessive sleepiness, which can severely affect their daily functioning. This excessive daytime sleepiness often leads to difficulty concentrating, memory problems, and a general feeling of fatigue. Morning headaches are another common symptom, resulting from the reduced oxygen levels during sleep. Additionally, irritability and mood changes can occur due to the lack of quality sleep.
Recognizing these symptoms and warning signs is essential. If you or a loved one exhibit any of these signs, it is important to seek medical advice. Early detection and treatment of sleep apnea can prevent complications such as cardiovascular issues, diabetes, and other serious health problems. A healthcare professional can conduct a thorough evaluation and recommend appropriate interventions to manage the condition effectively.
Understanding the symptoms and warning signs of sleep apnea enables individuals to take proactive steps towards better health. By addressing these issues promptly, one can improve sleep quality and overall life satisfaction, highlighting the importance of awareness and timely medical intervention.
Diagnosing sleep apnea involves a thorough and multi-faceted approach to ensure accurate identification of the disorder and appropriate treatment planning. The process typically begins with an initial medical consultation, where the healthcare provider reviews the patient’s medical history, symptoms, and risk factors. Common symptoms of sleep apnea include loud snoring, episodes of breathing cessation during sleep, and daytime fatigue. During this consultation, the physician may also conduct a physical examination to check for physical characteristics associated with sleep apnea, such as obesity, a large neck circumference, or enlarged tonsils.
One of the key diagnostic tools for sleep apnea is the sleep study, also known as polysomnography. This comprehensive test is usually conducted overnight in a sleep laboratory and monitors a variety of physiological parameters while the patient sleeps. These parameters include brain activity (electroencephalography), eye movements (electrooculography), muscle activity (electromyography), heart rate (electrocardiography), airflow, respiratory effort, and blood oxygen levels. The data collected from a polysomnography study can provide detailed insights into sleep stages, breathing patterns, and the frequency and severity of apnea events.
For some patients, a home sleep apnea test (HSAT) may be recommended as an alternative to in-lab polysomnography. HSATs are less comprehensive but more convenient, as they allow patients to undergo testing in the comfort of their own home. These tests typically measure fewer parameters, such as airflow, respiratory effort, and oxygen saturation. While HSATs can be effective in diagnosing moderate to severe sleep apnea, they may not be suitable for all patients, particularly those with complex medical conditions or suspected mild sleep apnea.
After the completion of the sleep study or HSAT, the collected data is analyzed by a sleep specialist. The results will indicate the presence and severity of sleep apnea, classified by the apnea-hypopnea index (AHI), which quantifies the number of apnea (complete cessation of airflow) and hypopnea (partial reduction in airflow) events per hour of sleep. Based on the AHI and other clinical findings, the healthcare provider will discuss the diagnosis with the patient and recommend an appropriate treatment plan.
Treatment Options
When it comes to managing sleep apnea, several treatment options are available, each with its own set of benefits and potential drawbacks. One of the first recommendations for individuals diagnosed with sleep apnea is to make specific lifestyle changes. Weight loss is often suggested, as excess weight can contribute to the narrowing of the airways. Additionally, quitting smoking is highly recommended, as smoking can increase inflammation and fluid retention in the upper airway.
Another common treatment option is the use of Continuous Positive Airway Pressure (CPAP) machines. CPAP devices work by delivering a steady stream of air through a mask, keeping the airways open during sleep. CPAP is highly effective and considered the gold standard for treating obstructive sleep apnea. However, some patients may find the masks uncomfortable or have difficulty adhering to the nightly use of the machine.
For those who cannot tolerate CPAP, oral appliances might be a suitable alternative. These devices are designed to keep the throat open by repositioning the jaw or tongue during sleep. Oral appliances can be particularly beneficial for individuals with mild to moderate sleep apnea. They are generally more comfortable than CPAP machines and easier to travel with. However, they may not be as effective for severe cases of sleep apnea and can cause jaw discomfort or dental issues over time.
Surgical interventions are also an option for treating sleep apnea, especially when other treatments have failed. Procedures can range from minimally invasive techniques, such as radiofrequency ablation, to more complex surgeries like uvulopalatopharyngoplasty (UPPP) or maxillomandibular advancement (MMA). Surgery can offer a permanent solution, but it carries the risks inherent to surgical procedures, including complications and varying success rates.
Ultimately, the choice of treatment depends on the severity of the condition, patient preferences, and the presence of any underlying health issues. Consulting with a healthcare provider is essential to determine the most appropriate treatment plan tailored to an individual’s specific needs.

Living with Sleep Apnea
Managing sleep apnea involves a multi-faceted approach that integrates lifestyle modifications, adherence to treatment plans, and coping strategies to improve quality of life for both patients and their families. Living with sleep apnea requires attention to various aspects of daily life to minimize symptoms and enhance overall well-being.
Maintaining a healthy lifestyle is paramount for individuals with sleep apnea. Regular physical activity can help manage body weight, a significant factor in mitigating the severity of sleep apnea. Incorporating a balanced diet, rich in fruits, vegetables, lean proteins, and whole grains, supports overall health and can contribute to weight management. Avoiding alcohol and sedatives, especially before bedtime, can also reduce sleep apnea episodes as these substances relax the muscles in the throat, exacerbating airway obstruction.
Adherence to prescribed treatment plans is crucial in managing sleep apnea effectively. Continuous Positive Airway Pressure (CPAP) therapy is commonly recommended and requires consistent use to be effective. Patients should ensure their CPAP devices are properly fitted and maintained. For those using oral appliances, regular adjustments and fittings are necessary. It is essential to follow the advice of healthcare providers regarding the use of any prescribed medications or therapies.
Coping strategies are vital for both patients and their families. Education about sleep apnea and its impact can help families provide better support. Establishing a regular sleep routine, including a consistent bedtime and wake-up time, can improve sleep quality. Creating a sleep-friendly environment by reducing noise, light, and maintaining a comfortable room temperature can further enhance sleep.
Regular follow-ups with healthcare providers are essential for monitoring the condition and making necessary adjustments to treatment plans. These appointments allow for the evaluation of the efficacy of current treatments and the exploration of new options if needed. Patients should communicate any changes in symptoms or new health concerns to their healthcare providers promptly.
FAQ : Understanding Sleep Apnea
What are the long-term effects of untreated sleep apnea?
Untreated sleep apnea can lead to several serious health complications over time. Individuals with untreated sleep apnea are at a higher risk of cardiovascular conditions like hypertension, heart attack, stroke, and arrhythmias. Moreover, it can exacerbate metabolic disorders such as type 2 diabetes. Mental health issues, including depression and anxiety, are also common among those with untreated sleep apnea. The chronic fatigue caused by disrupted sleep can impair cognitive functions, affecting memory, concentration, and overall quality of life.
How does sleep apnea affect different age groups?
Sleep apnea affects individuals of all ages, though the prevalence and impact may vary. In children, sleep apnea can cause behavioral problems, poor academic performance, and growth issues. Adults, particularly those who are overweight or have certain anatomical features, are at a higher risk of developing sleep apnea. In older adults, sleep apnea may present with more severe symptoms and is often associated with other comorbidities such as cardiovascular diseases and cognitive decline.
Is sleep apnea treatment covered by insurance?
Coverage for sleep apnea treatment varies by insurance provider and plan. Generally, most insurance plans, including Medicare, cover diagnosis and treatment options like CPAP therapy and oral appliances. However, coverage specifics can differ, so it is advisable to check with your insurance provider for detailed information. Additionally, some insurance plans may require prior authorization or a documented failure of conservative treatments before approving more advanced options.
What are the latest research developments in sleep apnea?
Recent research in sleep apnea has focused on improving diagnostic methods and treatment efficacy. Advances in home sleep testing have made diagnosis more accessible. Innovations in CPAP technology, such as auto-adjusting devices and more comfortable masks, have improved patient compliance. Research on alternative treatments, like hypoglossal nerve stimulation and pharmacotherapy, is ongoing. Additionally, studies are examining the genetic factors contributing to sleep apnea, aiming to develop personalized treatment approaches.
Can lifestyle changes help manage sleep apnea?
Yes, certain lifestyle changes can help alleviate the symptoms of sleep apnea, particularly in mild cases. Maintaining a healthy weight is one of the most effective ways to reduce sleep apnea severity. Regular physical activity, avoiding alcohol or sedatives close to bedtime, and sleeping on your side instead of your back can also help prevent airway obstruction. Smoking cessation is crucial, as smoking can increase inflammation and fluid retention in the upper airway, worsening sleep apnea. A consistent sleep routine and improving sleep hygiene can also support better sleep quality.
What are the signs that I may have sleep apnea?
Common signs of sleep apnea include loud snoring, choking or gasping for air during sleep, excessive daytime sleepiness, difficulty concentrating, and irritability. People with sleep apnea may also experience morning headaches or a dry mouth. If you have any of these symptoms, it’s important to consult with a healthcare professional for an evaluation and potential sleep study. Early detection and treatment can prevent the progression of the disorder and reduce the risk of complications.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

