Traumatic Sternal Bulge: Causes, Symptoms, and Treatment Options
The human chest is a robust structure that protects vital organs, including the heart. However, certain traumatic incidents can lead to injuries that may result in unique conditions, such as a traumatic sternal bulge. In this blog post, we will delve into the causes, symptoms, and treatment options for this less commonly known condition.
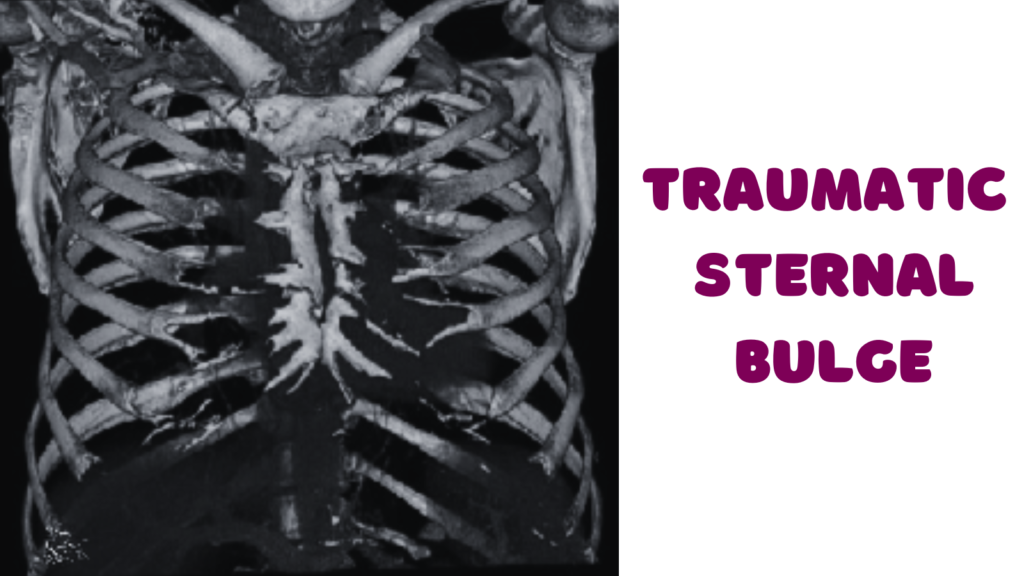
What is a Traumatic Sternal Bulge?
A traumatic sternal bulge occurs when there is a forceful impact to the chest, causing the sternum (breastbone) to deform or protrude abnormally. This can happen due to various traumatic events, such as car accidents, falls, or direct blows to the chest.
Causes of Traumatic Sternal Bulge
Here are some common causes of chest trauma that could result in sternal issues:
- Blunt Force Trauma: Direct impact to the chest, such as from a car accident, fall, or assault, can cause trauma to the sternum and surrounding structures.
- Sports Injuries: Athletes, particularly those engaged in contact sports like football or hockey, may experience chest trauma that could lead to sternal injuries.
- Falls: A fall onto the chest or a hard surface can cause significant trauma to the sternum.
- Industrial or Workplace Accidents: Accidents involving heavy machinery, falling objects, or other workplace incidents can result in chest injuries.
- Motor Vehicle Accidents: The force involved in car accidents, especially those with a front impact, can lead to chest trauma.
- Assaults or Physical Altercations: Physical altercations or assaults that involve blows to the chest can cause trauma to the sternum.
- Medical Procedures: In some cases, medical interventions or surgeries involving the chest may lead to complications, although this is less common.
Symptoms of Traumatic Sternal Bulge
While the term “traumatic sternal bulge” may not be a recognized medical term, if we consider symptoms related to chest trauma or injuries that could potentially lead to a sternal bulge, the following are some general symptoms that individuals might experience:
- Visible Deformity: A noticeable bulge, protrusion, or deformity in the chest region may be evident, indicating a potential issue with the sternum.
- Pain and Tenderness: Pain at the site of impact is a common symptom. The affected individual may experience tenderness, especially when touching or applying pressure to the chest.
- Difficulty Breathing: Severe chest trauma can affect the ability to breathe comfortably. Shortness of breath or difficulty taking deep breaths may occur.
- Bruising and Swelling: External signs of trauma, such as bruising and swelling, may be visible on the chest. This can indicate damage to blood vessels and soft tissues.
- Chest Pain: Pain in the chest, either localized or radiating, is a common symptom. The pain may worsen with movement or certain activities.
- Rib Fractures: Chest trauma can also lead to fractures of the ribs, and this may contribute to the overall discomfort and pain experienced.
- Crepitus: A grating or cracking sensation (crepitus) may be felt or heard at the site of injury, particularly if there is bone involvement.
It’s important to note that symptoms can vary in severity depending on the nature and extent of the chest trauma. Additionally, internal injuries may not always be immediately visible, so any concerns regarding chest trauma should prompt a prompt medical evaluation.
Diagnosis
The diagnosis of a traumatic sternal bulge or any chest trauma-related condition typically involves a thorough medical evaluation, physical examination, and sometimes imaging studies. Here’s an overview of the diagnostic process:
- Medical History: The healthcare provider will begin by taking a detailed medical history, including information about the circumstances leading to the chest trauma, the nature of the impact, and any symptoms experienced.
- Physical Examination: A careful physical examination is conducted to assess the chest area. The healthcare provider will look for signs of deformity, tenderness, bruising, swelling, and any other visible abnormalities. They may also assess breathing patterns and listen to the chest with a stethoscope.
- Imaging Studies:
- X-rays: X-rays are commonly used to visualize the bones of the chest, including the sternum and ribs. X-rays can help identify fractures, dislocations, or other skeletal abnormalities.
- Computed Tomography (CT) Scan: In cases where more detailed imaging is needed, a CT scan may be ordered. CT scans provide cross-sectional images of the chest, offering a more comprehensive view of the structures involved.
- Ultrasound: In some situations, an ultrasound may be used to assess soft tissues and detect any abnormalities or fluid collections in the chest.
- Magnetic Resonance Imaging (MRI): While less commonly used for chest trauma, an MRI may be employed to evaluate soft tissues and provide additional information about the extent of the injury.
- Laboratory Tests: Blood tests may be ordered to assess for signs of internal injuries, such as bleeding or inflammation.
- Pulmonary Function Tests: In cases where there is concern about the impact on respiratory function, pulmonary function tests may be conducted to assess lung capacity and function.
- Electrocardiogram (ECG or EKG): If there is a risk of cardiac involvement due to the chest trauma, an electrocardiogram may be performed to assess the heart’s electrical activity.
The combination of these diagnostic tools allows healthcare professionals to accurately assess the extent of the chest trauma, identify any fractures or deformities, and formulate an appropriate treatment plan. The diagnostic approach may vary based on the specific circumstances and severity of the traumatic sternal bulge or chest injury.
Treatment Options
The approach to treating a traumatic sternal bulge depends on the severity of the injury. Mild cases may be managed with pain medications, rest, and close monitoring. However, more severe cases may require surgical intervention to realign the sternum and stabilize the chest wall.
The treatment of a traumatic sternal bulge or chest trauma depends on the severity of the injury. Mild cases may be managed with conservative measures, while more severe injuries may require surgical intervention. Here are some general approaches to treatment:
Conservative Treatment:
- Pain Management:
- Over-the-counter pain relievers (such as acetaminophen or ibuprofen) or prescription medications may be recommended to manage pain.
- Rest and Immobilization:
- Adequate rest is crucial for the healing process. Restricting activities that strain the chest muscles helps prevent further injury.
- Ice Packs:
- Applying ice packs to the affected area can help reduce swelling and alleviate pain. However, it’s essential to use a cloth or towel to avoid direct contact with the skin.
- Monitoring:
- Regular monitoring by a healthcare professional is essential to track the progress of the healing process and identify any complications.
Surgical Treatment:
- Closed Reduction:
- In cases where there is a dislocation or misalignment of the sternum, closed reduction may be performed. This involves manipulating the bones back into their proper position without surgery.
- Open Reduction and Internal Fixation (ORIF):
- For more severe sternal fractures or deformities, surgical intervention may be necessary. Surgeons may use fixation devices such as wires, plates, or screws to stabilize the sternum and facilitate proper healing.
- Repair of Associated Injuries:
- If there are other injuries to the chest, ribs, or internal organs, surgical repair may be required.
Rehabilitation:
- Physical Therapy:
- Physical therapy may be prescribed to promote mobility, strengthen the chest muscles, and prevent stiffness. Therapists can provide exercises and guidance tailored to the individual’s condition.
- Breathing Exercises:
- In cases where there is difficulty breathing, respiratory exercises may be recommended to improve lung function and prevent complications like pneumonia.
Follow-Up Care:
- Regular Check-ups:
- Follow-up appointments with healthcare providers are crucial to monitor the healing process, assess for any complications, and adjust the treatment plan as needed.
- Activity Graduation:
- Returning to regular activities should be gradual and guided by healthcare professionals to prevent re-injury.
Emergency Situations:
If there are signs of severe chest trauma, difficulty breathing, or other life-threatening symptoms, emergency medical attention should be sought immediately.
Recovery Process
Recovery from a traumatic sternal bulge or chest trauma varies depending on the severity of the injury, the type of treatment received, and individual factors. Here are general considerations for the recovery process:
Early Recovery (First Few Weeks):
- Pain Management:
- Pain is often most pronounced in the early stages of recovery. Medications prescribed by healthcare providers can help manage pain and discomfort.
- Rest and Immobilization:
- Adequate rest is crucial during the initial recovery period. Immobilization of the chest through bracing or avoiding certain movements may be recommended.
- Follow-Up Appointments:
- Regular follow-up appointments with healthcare professionals are essential to monitor the progress of healing, address any concerns, and make adjustments to the treatment plan if necessary.
Intermediate Recovery (Weeks to Months):
- Physical Therapy:
- As the initial pain subsides, physical therapy may be introduced to promote mobility and prevent stiffness. Therapists will guide patients through exercises to strengthen the chest muscles and improve flexibility.
- Gradual Resumption of Activities:
- Return to normal activities should be gradual and guided by healthcare professionals to prevent re-injury. Patients may be advised to avoid certain movements or activities during this phase.
- Monitoring for Complications:
- Healthcare providers will continue to monitor for any signs of complications, such as infection, and address them promptly.
Long-Term Recovery (Months to a Year or Longer):
- Full Rehabilitation:
- Complete rehabilitation may take several months, particularly for more severe injuries. Continued physical therapy or home exercises may be necessary to achieve optimal strength and flexibility.
- Pain Resolution:
- Pain should progressively diminish over time. If pain persists or worsens, it is crucial to consult with healthcare providers for further evaluation.
- Resumption of Normal Activities:
- Patients can gradually resume normal activities and exercises, keeping in mind any recommendations or restrictions provided by healthcare professionals.
- Follow-Up Assessments:
- Periodic follow-up assessments may be scheduled to monitor long-term recovery and address any lingering issues.
Psychological Support:
Recovery from chest trauma is not only physical but can also involve emotional and psychological aspects. Patients may experience anxiety, fear, or stress during the recovery process. Psychological support, counseling, or support groups can be valuable resources for individuals coping with the emotional impact of a traumatic event.
Warning Signs:
Patients should seek medical attention if they experience any of the following:
- Increasing pain or discomfort
- New or worsening symptoms
- Signs of infection (such as redness, swelling, or drainage at the site)
- Difficulty breathing or chest pain
Recovery is highly individual, and the timeline can vary. It’s essential for patients to follow their healthcare provider’s advice, adhere to prescribed treatments, and communicate any concerns or changes in their condition throughout the recovery journey.
Disclaimer
This blog post is intended for informational purposes only and should not be considered as medical advice. It is crucial to consult with a qualified healthcare professional for accurate diagnosis, treatment options, and personalized medical guidance based on individual circumstances. The information provided in this post is based on general knowledge and may not reflect the latest advancements or specific medical conditions.
Stay updated—subscribe now for informed empowerment!

