Vestibulocochlear Nerve: 7 Shocking Facts Revealed
Vestibulocochlear Nerve
The vestibulocochlear nerve, known scientifically as cranial nerve VIII, plays a crucial role in our sensory systems, specifically in auditory and vestibular functions. This nerve is responsible for transmitting sound information from the cochlea to the brain, where it is processed and interpreted, allowing individuals to perceive sound. Additionally, it plays a vital role in maintaining balance and spatial orientation through its vestibular component, which detects changes in the position and motion of the head.
Sign up for HUMANITYUAPD
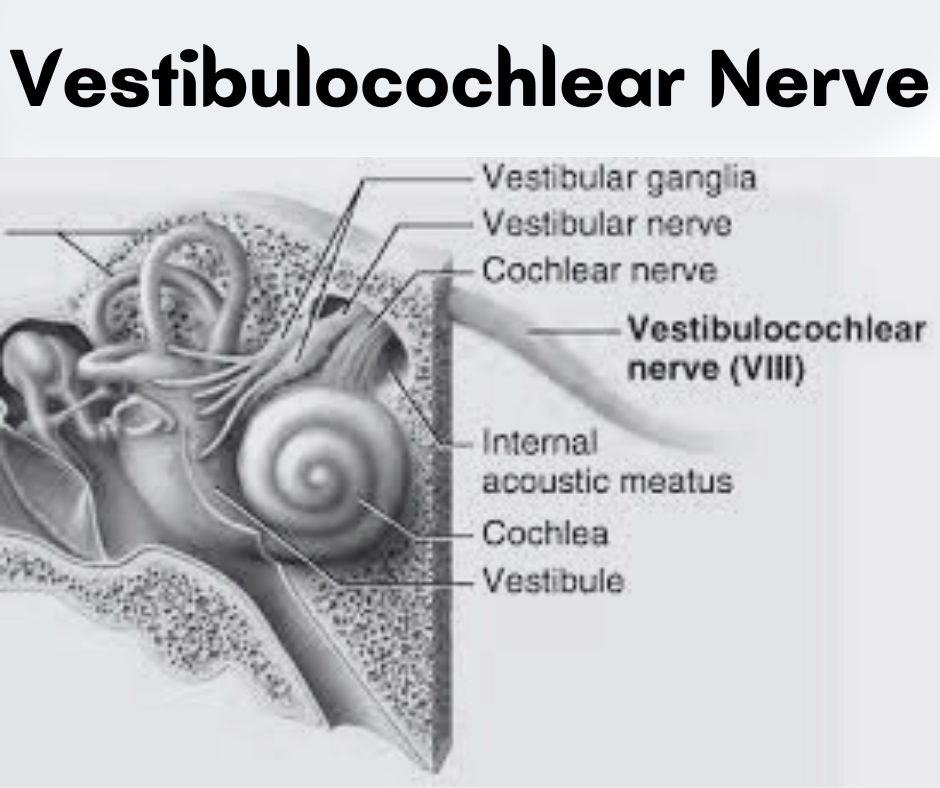
Anatomically, the vestibulocochlear nerve emerges from the brainstem at the level of the pons. It consists of two main branches: the cochlear branch, which carries auditory information, and the vestibular branch, responsible for balance-related information. Each branch has a distinct pathway; the cochlear fibers travel from the cochlea through the internal auditory canal to reach the cochlear nuclei in the brainstem, while the vestibular fibers originate from the semicircular canals and the otolith organs of the inner ear, relaying information to the vestibular nuclei.
The significance of the vestibulocochlear nerve transcends mere auditory perception and balance. It acts as a conduit that integrates sensory information, enabling the body to respond effectively to changes in the environment. Any impairment in this nerve can lead to disorders such as hearing loss, tinnitus, vertigo, or balance issues. Understanding the structure and function of the vestibulocochlear nerve is essential for recognizing the importance of auditory and vestibular health, laying the groundwork for further exploration into its functions, disorders, and potential treatments.
➡️ Table of Contents ⬇️
Anatomy of the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as cranial nerve VIII, is a critical component of the auditory and balance systems within the human body. It primarily serves two essential functions, encompassing both hearing and equilibrium. Anatomically, the nerve can be divided into two distinct branches: the cochlear branch and the vestibular branch. These branches originate from the inner ear and transmit sensory information to the brain.
The cochlear branch is responsible for hearing. It arises from the spiral ganglion located in the cochlea, where it collects auditory information. This branch then extends toward the brainstem, where it synapses at the cochlear nuclei. In contrast, the vestibular branch is associated with balance. This branch is linked to structures such as the semicircular canals and otolith organs, which detect changes in head position and motion. The vestibular branch’s sensory neurons originate from the vestibular ganglion, transmitting information to the brainstem, particularly the vestibular nuclei.
This intricate anatomical configuration is heavily intertwined with other cranial nerves and neural pathways. Its relations to cranial nerves VII, IX, and X exemplify the complex communication network responsible for sensory integration. Additionally, diagrams of the anatomy of the vestibulocochlear nerve are invaluable resources for visualizing its pathways and connections, helping to clarify its anatomical position relative to the inner ear structures and central nervous system.
Overall, understanding the vestibulocochlear nerve’s anatomy is fundamental for comprehending its essential roles in both hearing and balance. Further exploration of this subject can reveal the complexities of how sensory information is processed and utilized by the body.
Functions of the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as cranial nerve VIII, is crucial for two primary functions: hearing and balance. These functions are facilitated through the transmission of sensory information from the inner ear to specific areas in the brain. Understanding how these processes work provides insight into the importance of this nerve in everyday life.
In terms of hearing, the vestibulocochlear nerve transmits sound signals from the cochlea, a spiral-shaped organ in the inner ear. The cochlea is lined with hair cells that respond to sound waves by converting them into electrical signals. These signals are subsequently sent through the vestibulocochlear nerve to the brainstem, where they are routed to the auditory cortex in the temporal lobe of the brain. This pathway ensures that auditory information is processed efficiently, allowing for sound perception and interpretation. The hair cells play a critical role, as they are responsible for detecting sound frequencies and intensities, enabling individuals to perceive a wide range of sounds.
On the other hand, the balance function of the vestibulocochlear nerve is associated with the vestibular system. This system includes the semicircular canals and otolith organs, which detect changes in head position and motion. The hair cells within these structures transduce mechanical movements into neural signals, which are communicated through the vestibulocochlear nerve to the vestibular nuclei in the brainstem. From there, information is integrated to maintain equilibrium and stabilize posture.
This process is essential for everyday activities, such as walking, running, and maintaining a steady gaze while in motion. Together, the functions of hearing and balance illustrate the integral role of the vestibulocochlear nerve in sensory processing and coordination, thereby contributing to an individual’s overall perception and interaction with their environment.

Clinical Significance of the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as cranial nerve VIII, plays a critical role in our auditory and vestibular systems, linking the inner ear to the brain. Dysfunction of this nerve can lead to a variety of clinical conditions, most notably hearing loss, tinnitus, vertigo, and Meniere’s disease. Early recognition and accurate diagnosis of these disorders are essential for effective management and patient care.
Hearing loss can manifest as a gradual decline in auditory perception or sudden, complete deafness. Conductive hearing loss, often due to middle ear issues, may temporarily obscure the vital functions of the vestibulocochlear nerve. Sensorineural hearing loss, however, results from direct damage to the nerve or inner ear structures, frequently linked to aging, exposure to loud noise, or ototoxic medications. Timely audiological assessments can help determine the specific type of hearing loss and direct subsequent therapeutic interventions.
Tinnitus, characterized by the perception of ringing or buzzing without external sound stimuli, is another common issue connected with vestibulocochlear nerve dysfunction. Lasting effects of tinnitus can lead to significant distress, affecting quality of life. Various treatment options, such as sound therapy or cognitive behavioral therapy, can provide relief and are initiated through professional diagnosis.
Vertigo, a sensation of spinning or dizziness, can also be a consequence of vestibulocochlear nerve impairment. It often signals underlying vestibular dysfunction, with diagnostic methods including vestibular evoked myogenic potentials and caloric testing. This information can guide effective management strategies aimed at restoring balance and mitigating symptoms.
Lastly, Meniere’s disease, a complex condition marked by episodes of vertigo, hearing fluctuations, and aural fullness, is also associated with vestibulocochlear nerve issues. Given its unpredictable and recurrent nature, ongoing monitoring and tailored treatment plans become integral to managing this chronic disorder.
Testing the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as cranial nerve VIII, plays a critical role in both hearing and balance. To assess its integrity and functional capacity, healthcare professionals utilize several diagnostic tests. Among the most common are audiometry, electronystagmography (ENG), and tuning fork tests, each serving a distinct purpose in evaluating this complex nerve.
Audiometry is often the first test performed to evaluate hearing function. This test typically includes pure-tone audiometry, which measures a patient’s ability to hear different frequencies at varying intensities. Patients wear headphones and respond to sounds played at various pitches and volumes. The results are plotted on an audiogram, where specific thresholds indicate normal hearing, conductive hearing loss, or sensorineural hearing loss, thus providing insights into the cochlear function of the vestibulocochlear nerve.
Electronystagmography is another crucial test, primarily focused on assessing balance. This technique measures eye movements in response to stimuli, as the vestibular system is closely linked to eye reflexes. During ENG, electrodes are placed around the eyes to record eye positions while the patient undergoes a series of head movements and caloric tests. Abnormal findings may indicate vestibular dysfunction, suggesting that the vestibulocochlear nerve is not functioning properly in relaying equilibrium information to the brain.
Tuning fork tests, like the Rinne and Weber tests, serve as simple yet effective methods to differentiate types of hearing loss. A vibrating tuning fork is placed on the mastoid bone or in front of the ear. The patient’s perception of sound through air versus bone conduction helps determine whether hearing loss is conductive or sensorineural in nature. These assessments are essential for evaluating the status of the vestibulocochlear nerve and guide further diagnostic and therapeutic steps.
Treatment Options for Vestibulocochlear Nerve Disorders
The management of disorders associated with the vestibulocochlear nerve, also known as cranial nerve VIII, requires a multifaceted approach tailored to the underlying condition and specific patient needs. Treatment options can broadly be categorized into pharmaceutical interventions, rehabilitation techniques, and surgical procedures.
Pharmaceutical interventions typically involve the use of medications to alleviate symptoms or address the underlying pathology. For instance, vestibular suppressants such as meclizine or diazepam may be prescribed to manage vertigo or dizziness. Additionally, corticosteroids may be utilized to reduce inflammation in conditions like vestibular neuritis, which can help restore function and diminish symptoms. It is essential for healthcare providers to monitor and adjust these medications based on patient response and any potential side effects.
Another significant aspect of treatment is rehabilitation therapy, particularly vestibular therapy. This type of rehabilitation focuses on exercises designed to improve balance and reduce dizziness. Patients work with trained physical therapists who employ specific maneuvers to promote the central nervous system’s adaptation to vestibular loss. Techniques such as gaze stabilization exercises and habituation can significantly enhance functional outcomes and quality of life for individuals suffering from vestibular disorders.
In cases where conservative management is insufficient, surgical options may be considered. Surgical interventions are usually reserved for more severe conditions, such as acoustic neuroma or Meniere’s disease, where there is a significant impact on patient functionality. Surgical removal of tumors or the resection of vestibular nerves can provide relief, albeit with associated risks and varying degrees of success.
Ultimately, the selection of treatment needs to be individualized, taking into account the specific disorder, its severity, and the overall health of the patient. In addressing vestibulocochlear nerve disorders, a comprehensive strategy can substantially enhance patient outcomes and improve quality of life.

Vestibulocochlear Nerve and Aging
The vestibulocochlear nerve, also known as cranial nerve VIII, plays a pivotal role in both hearing and balance. As individuals age, this nerve can be adversely affected, often leading to a range of auditory and vestibular disorders. Age-related changes in the inner ear structures directly influence the functioning of the vestibulocochlear nerve, resulting in common ailments such as presbycusis, a type of age-related hearing loss characterized by a gradual decline in the ability to perceive high-frequency sounds.
In addition to auditory deficits, the vestibulocochlear nerve is integral to maintaining balance. Aging can lead to a deterioration of the vestibular apparatus located in the inner ear, which is instrumental in spatial awareness and orientation. This deterioration often manifests as increased instances of dizziness or imbalance among older adults, which raises concern given the potential for falls. The connection between balance disorders and the functionality of the vestibulocochlear nerve underscores the importance of maintaining vestibular health as one ages.
Various preventative measures can be adopted to alleviate the adverse effects associated with aging and the vestibulocochlear nerve. Regular physical activity is essential; it promotes overall health, enhances balance, and may help maintain vestibular function. Additionally, engaging in exercises specifically aimed at improving balance, such as tai chi or yoga, can be beneficial. Furthermore, routine hearing assessments allow for early detection of any changes in hearing ability, facilitating timely interventions, such as hearing aids or therapeutic options. Nutrition also plays a crucial role, with a diet rich in antioxidants and vitamins potentially supporting nerve health.
Ultimately, understanding the relationship between aging and the vestibulocochlear nerve is vital. This knowledge empowers individuals and healthcare professionals to adopt proactive strategies to maintain auditory and vestibular function, thereby enhancing quality of life as one ages.
FAQs about the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as cranial nerve VIII, plays a crucial role in our ability to hear and maintain balance. Many individuals have questions regarding its functions, associated symptoms, and treatments for dysfunction. Below are some frequently asked questions that encapsulate key information pertinent to the vestibulocochlear nerve.
What symptoms indicate vestibulocochlear nerve dysfunction?
Common symptoms include hearing loss, tinnitus (ringing in the ears), dizziness, and balance problems. Patients may experience these symptoms simultaneously or in isolation. Hearing loss can occur suddenly or progressively, and balance issues may manifest as vertigo, unsteadiness, or a sensation of spinning.
What are the causes of vestibulocochlear nerve impairment?
Dysfunction can arise from various conditions such as acoustic neuromas, infections, head trauma, or labyrinthitis. In some cases, exposure to loud noises may also damage this nerve, leading to hearing impairment. Understanding the underlying cause is essential for determining the appropriate course of treatment.
How is vestibulocochlear nerve dysfunction diagnosed?
Diagnosis typically involves a comprehensive evaluation that may include hearing tests, balance assessments, and imaging studies like MRI scans. Healthcare professionals use these tools to ascertain the condition of the vestibulocochlear nerve and to rule out other potential causes of the symptoms.
What treatment options are available?
Treatment depends on the underlying cause of the dysfunction. Options may range from medication to relieve symptoms, such as vertigo, to surgical interventions for structural problems. Hearing aids may be recommended for those experiencing significant hearing loss. Rehabilitation therapies aimed at re-establishing balance may also be beneficial.
Can vestibulocochlear nerve damage be reversed?
The potential for recovery depends on the cause and severity of the damage. In some cases, such as mild viral infections, function may improve over time. However, permanent damage from conditions like acoustic neuromas or prolonged exposure to loud noise is typically irreversible. Treatments like hearing aids, cochlear implants, or vestibular rehabilitation can help manage symptoms and improve quality of life.
Awareness and understanding of the vestibulocochlear nerve can significantly enhance patient outcomes. If symptoms arise, early consultation with healthcare professionals is advisable to explore potential interventions.
Conclusion
In short, the vestibulocochlear nerve, also known as cranial nerve VIII, plays a vital role in both hearing and balance. Understanding its anatomy and functionality is essential for medical professionals engaged in diagnosing and treating related disorders. This nerve is divided into two components: the cochlear nerve, responsible for transmitting auditory information, and the vestibular nerve, which manages balance and spatial orientation. Given the intertwining of these functions, any dysfunction can lead to significant impacts on an individual’s quality of life.
Throughout this comprehensive guide, we have explored various aspects of the vestibulocochlear nerve, including its pathway, associated conditions, and the diagnostic methods used to assess its integrity. Disorders such as vestibular neuritis, Meniere’s disease, and acoustic neuromas highlight the importance of prompt recognition and treatment. Individuals experiencing symptoms such as hearing loss, vertigo, or tinnitus are encouraged to seek professional evaluation to determine the underlying cause and appropriate course of action.
Moreover, ongoing research continues to unveil the complexities of the vestibulocochlear nerve and its implications on auditory and vestibular health. Advancements in medical technology and methodologies promise to enhance our understanding of this critical nerve, which can lead to improved treatment options for patients. The necessity for awareness concerning the vestibulocochlear nerve is paramount, not only for healthcare providers but also for individuals to recognize when to seek care. Emphasizing the significance of both preventative measures and tailored treatments can ultimately promote better health outcomes and enhance the overall well-being of those affected by vestibular and auditory conditions.

Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

