Costochondritis: Understanding and Managing Chest Pain
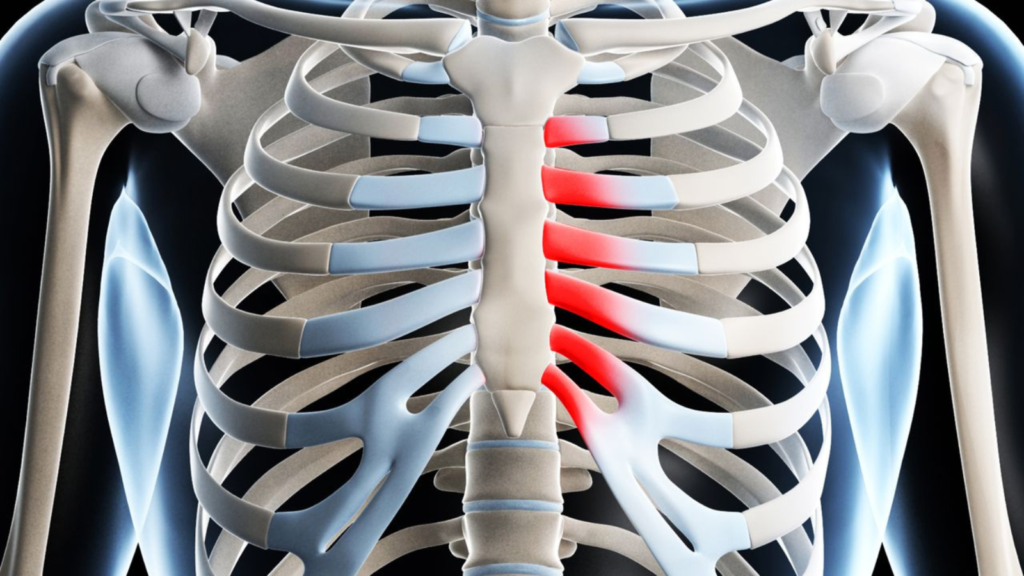
Costochondritis is a common but often misunderstood condition that affects the cartilage where the upper ribs attach to the sternum, an area known as the costosternal junction. This condition can cause chest pain and discomfort, leading many individuals to become concerned about more serious cardiac issues. In this blog post, we will explore the various aspects of costochondritis, including its causes, symptoms, and management strategies.
What is Costochondritis?
Costochondritis is a condition that causes inflammation and pain in the cartilage that connects the ribs to the breastbone. It can sometimes be mistaken for a heart attack or other serious problems, but it is usually harmless and goes away on its own. Here are some facts about costochondritis that you might find useful:
- Costochondritis can affect anyone, but it is more common in women and people older than 40 years.
- The exact cause of costochondritis is unknown, but it may be related to injury, physical strain, infection, arthritis, or genetic factors.
- The main symptom of costochondritis is chest pain that is sharp, dull, or pressure-like. It usually occurs on the left side of the chest, but it can also affect both sides or the right side. The pain may worsen with breathing, coughing, sneezing, or movement of the chest or arms.
- Costochondritis is diagnosed by a physical examination, where the doctor will check for tenderness and swelling at the junctions of the ribs and the breastbone. Other tests, such as blood tests, X-rays, or electrocardiograms, may be done to rule out other causes of chest pain.
- Costochondritis is treated with pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), narcotics, antidepressants, or anti-seizure drugs. Some people may also benefit from physical therapy, such as stretching exercises or nerve stimulation. In rare cases, injections of numbing medication and corticosteroids may be given to the affected area.
- Costochondritis usually improves within a few weeks or months, but some people may have chronic pain that lasts longer. To prevent or reduce the risk of costochondritis, it is advisable to rest, use heat or cold therapy, avoid heavy lifting or strenuous exercise, treat infections promptly, and use backpacks properly.
Causes of Costochondritis
The exact cause of costochondritis is often unclear, and in many cases, it may develop without a specific identifiable reason. However, several factors and potential triggers have been associated with the development of costochondritis. Some of the common causes and contributing factors include:
- Physical Strain and Overuse: Excessive physical activity or strain, especially in the upper body, can lead to overuse of the chest muscles and strain on the cartilage in the costosternal junction or between the ribs.
- Injury or Trauma: Direct trauma to the chest, such as a fall, a blow to the chest, or a car accident, can cause damage to the cartilage and lead to inflammation.
- Repetitive Movements: Certain occupations or activities that involve repetitive movements of the upper body, such as heavy lifting or pushing, may increase the risk of developing costochondritis.
- Joint Infections: Although rare, infections affecting the costosternal or costovertebral joints can result in inflammation of the cartilage.
- Underlying Inflammatory Conditions: Conditions like rheumatoid arthritis or ankylosing spondylitis, which involve inflammation of the joints, may contribute to the development of costochondritis.
- Respiratory Infections: Viral or bacterial respiratory infections, such as a severe cough or bronchitis, can sometimes trigger inflammation in the chest area.
- Post-Surgery: In some cases, surgical procedures involving the chest or upper body may lead to the development of costochondritis.
- Costosternal Syndrome: This is a term sometimes used to describe a condition where there is inflammation of the costosternal junction without a clear underlying cause.
What are the symptoms of costochondritis?
The primary symptom of costochondritis is chest pain, and the condition can mimic the symptoms of more serious cardiac issues. Here are the common symptoms associated with costochondritis:
- Chest Pain: The hallmark symptom of costochondritis is chest pain, which may vary in intensity. The pain is often described as sharp or aching and is typically located on the front of the chest, near the sternum. The pain may be on one side or both sides of the chest.
- Localized Tenderness: Pressing on the affected area may reveal tenderness and discomfort. The pain is often reproducible by palpating the costosternal junctions or costovertebral joints.
- Worsening Pain with Movement: Physical activities, movements, or deep breaths can exacerbate the chest pain associated with costochondritis. Patients may notice increased discomfort when performing activities that involve the chest muscles.
- Pain Radiation: While the pain is primarily concentrated in the chest area, it may radiate to the back or abdomen. This radiation is often a key factor in distinguishing costochondritis from more serious cardiac issues.
- Swelling and Inflammation: In some cases, there may be mild swelling and redness around the costosternal or costovertebral joints. However, visible signs of inflammation are not always present.
- Pain Reproduction by Pressing on the Chest: Healthcare providers may perform a physical examination to reproduce or intensify the pain by pressing on specific points along the costosternal or costovertebral junctions.
Diagnosis and Differentiation
Diagnosing costochondritis involves a combination of clinical evaluation, medical history review, and, if necessary, diagnostic tests to rule out other potential causes of chest pain. It’s crucial to differentiate costochondritis from more serious conditions, such as heart-related issues, as the symptoms can sometimes overlap. Here’s an overview of the diagnosis and differentiation process:
Diagnosis:
- Medical History:
- The healthcare provider will start by taking a detailed medical history, including information about the onset, duration, and characteristics of the chest pain.
- Any recent injuries, physical activities, or respiratory infections may be discussed to identify potential triggers.
- Physical Examination:
- A physical examination is a key component of the diagnostic process. The healthcare provider will palpate (press on) the chest to identify areas of tenderness or reproduce the pain.
- Tenderness and pain localized to the costosternal or costovertebral joints are indicative of costochondritis.
- Imaging Studies:
- While costochondritis is primarily a clinical diagnosis, imaging studies may be recommended to rule out other potential causes of chest pain.
- X-rays may be used to visualize the ribs and costosternal junctions. However, X-rays may not always show inflammation.
- In some cases, more advanced imaging techniques like MRI or CT scans may be ordered to get a clearer view of the cartilage and surrounding structures.
Differentiation from Other Conditions:
- Cardiac Issues:
- Differentiating costochondritis from cardiac issues is crucial. Tests like electrocardiogram (ECG or EKG), stress tests, and cardiac enzyme tests may be conducted to assess heart health and rule out conditions like angina or myocardial infarction.
- Gastrointestinal Issues:
- Conditions like gastroesophageal reflux disease (GERD) or peptic ulcers can also cause chest pain. Evaluating symptoms related to digestion and conducting tests like upper endoscopy may be necessary.
- Musculoskeletal Issues:
- Other musculoskeletal conditions, such as rib fractures or muscle strains, may mimic the symptoms of costochondritis. Imaging studies can help differentiate these conditions.
- Pulmonary Issues:
- Respiratory conditions like pleurisy or pneumonia may cause chest pain. Chest X-rays and respiratory function tests may be used to evaluate lung health.
- Psychological Factors:
- Stress and anxiety can contribute to chest pain. A thorough assessment of psychological factors may be considered in the diagnostic process.
It’s important for individuals experiencing chest pain, especially if it is severe or persistent, to seek prompt medical attention. While costochondritis is generally a benign condition, ruling out other potential causes ensures an accurate diagnosis and appropriate management. Healthcare providers use a comprehensive approach to consider various factors and perform the necessary tests to arrive at the correct diagnosis.
Managing Costochondritis
Managing costochondritis typically involves a combination of self-care measures, lifestyle adjustments, and, in some cases, medical interventions. Here are some strategies for managing costochondritis:
1. Pain Relief Medications:
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help reduce pain and inflammation. Acetaminophen may be used for pain relief as well.
2. Rest and Avoidance of Triggers:
- Rest: Giving the affected area time to heal is important. Avoid activities that may exacerbate symptoms, such as heavy lifting or strenuous exercise.
3. Heat or Cold Therapy:
- Heat Packs: Applying a heat pack to the affected area can help relax muscles and reduce inflammation.
- Cold Packs: Cold packs can be used to numb the area and provide relief from pain and swelling.
4. Physical Therapy:
- A physical therapist can provide exercises to improve posture, strengthen muscles, and increase flexibility. These exercises can help reduce strain on the chest muscles and joints.
5. Stress Management:
- Stress can exacerbate symptoms. Engaging in stress-reducing activities such as deep breathing, meditation, or yoga may be beneficial.
6. Posture Correction:
- Maintaining good posture can help alleviate strain on the chest muscles and joints. Ergonomic adjustments at work or home may be recommended.
7. Medication Adjustment:
- If costochondritis is related to an underlying inflammatory condition, your healthcare provider may adjust existing medications or prescribe anti-inflammatory drugs.
8. Corticosteroid Injections:
- In some cases, corticosteroid injections may be considered to reduce inflammation and provide temporary relief. This is typically done under the guidance of a healthcare professional.
9. Supportive Measures:
- Bracing or Taping: In certain cases, wearing a brace or using taping techniques may provide support to the chest area and alleviate symptoms.
10. Regular Follow-ups:
- Regular follow-up appointments with a healthcare provider are important to monitor progress and make adjustments to the management plan as needed.
When to Seek Medical Attention
While costochondritis is generally considered a benign and self-limiting condition, there are situations in which individuals should seek prompt medical attention. It’s important to distinguish costochondritis from more serious conditions that can cause chest pain. Here are instances when seeking medical attention is warranted:
- Severe or Persistent Chest Pain:
- If the chest pain is severe, persistent, or worsening over time, it is essential to seek immediate medical attention. Severe chest pain can be indicative of more serious conditions, such as a heart attack.
- Difficulty Breathing:
- Chest pain accompanied by difficulty breathing or shortness of breath should be evaluated promptly. Respiratory distress may indicate a more critical issue.
- Radiating Pain:
- If the chest pain radiates to the arms, neck, jaw, or back, it may be a sign of a cardiac issue. Seek emergency medical attention if you experience pain spreading to these areas.
- Swelling, Redness, or Warmth:
- If there is noticeable swelling, redness, or warmth in the chest area, it could suggest an inflammatory or infectious process requiring medical evaluation.
- Associated Symptoms:
- Symptoms such as nausea, vomiting, dizziness, or fainting in conjunction with chest pain may indicate a more urgent medical situation and should not be ignored.
- New or Unexplained Symptoms:
- If you are experiencing chest pain for the first time or if the symptoms are new and unexplained, it is crucial to seek medical attention to determine the cause.
- Previous Heart Conditions:
- Individuals with a history of heart conditions or cardiovascular risk factors should be especially vigilant and seek medical help if they experience chest pain.
- Pain Persisting Despite Rest and Medications:
- If rest, over-the-counter pain medications, and other self-care measures do not provide relief, it’s important to consult with a healthcare professional.
Remember that chest pain can have various causes, and while costochondritis is one potential explanation, ruling out more serious conditions is paramount. If in doubt, it is always safer to err on the side of caution and seek medical attention promptly. Emergency services should be contacted if there is any suspicion of a heart attack or another life-threatening condition. Only a healthcare professional can provide a thorough evaluation, conduct necessary tests, and determine the appropriate course of action based on the individual’s specific situation.
Disclaimer
The information provided in this blog post is for informational purposes only and should not be considered as medical advice. It is not intended to replace professional medical diagnosis, treatment, or guidance. Always seek the advice of your physician or qualified healthcare provider regarding any medical condition. If you are experiencing chest pain or other concerning symptoms, seek immediate medical attention. The author and publisher of this content are not responsible for any actions or decisions based on the information provided.
Stay updated—subscribe now for informed empowerment!

