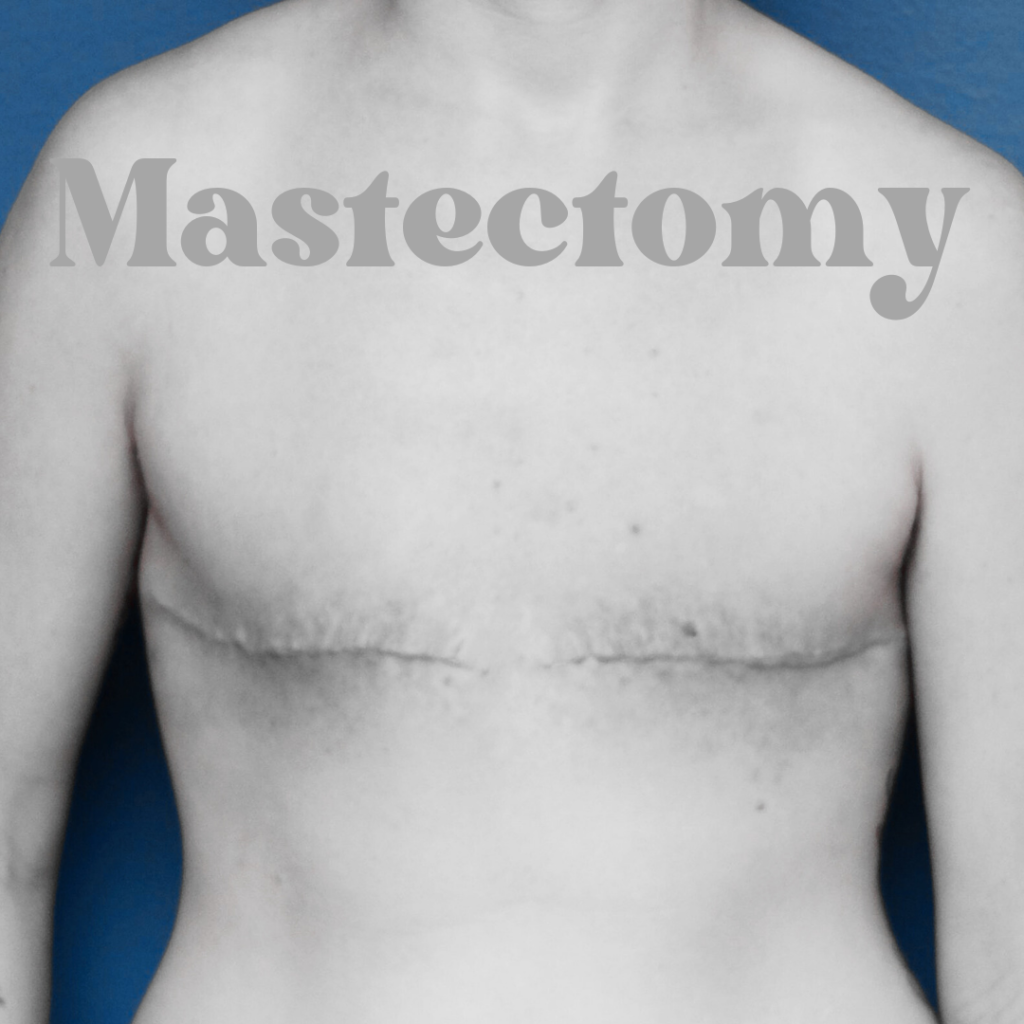
Mastectomy: Types, Emotional Considerations, and Recovery
Facing a mastectomy can be a challenging and emotional journey for anyone, regardless of the reason for the surgery. Whether you’re dealing with breast cancer, a genetic predisposition to the disease, or any other medical issue that requires breast removal, it’s essential to understand the procedure and the recovery process. In this blog post, we’ll discuss mastectomy, its types, and the steps to take for a successful post-surgery recovery.
Understanding Mastectomy
Mastectomy is a surgical procedure that involves the removal of one or both breasts. There are several types of mastectomy, each with its own specific characteristics. The choice of mastectomy type depends on various factors, including the stage of breast cancer, individual preferences, and the need for breast reconstruction. Here are the common types of mastectomy:
- Total Mastectomy (Simple Mastectomy): In a total mastectomy, the entire breast is removed, including the breast tissue, nipple, and areola. The underlying chest muscles are typically left intact. This procedure is often recommended for early-stage breast cancer or when the goal is to remove the entire breast while preserving the chest muscles.
- Modified Radical Mastectomy: This type of mastectomy involves the removal of the entire breast, as in a total mastectomy, but it also includes the removal of some lymph nodes in the underarm area (axillary lymph nodes) and the lining over the chest muscles. It is commonly recommended for more advanced stages of breast cancer.
- Double (Bilateral) Mastectomy: In a bilateral mastectomy, both breasts are removed. This choice is typically made by individuals who have a high risk of developing breast cancer, such as those with a strong family history of the disease or specific genetic mutations (e.g., BRCA1 or BRCA2).
- Skin-Sparing Mastectomy: Skin-sparing mastectomy aims to preserve as much of the breast skin as possible. The breast tissue, nipple, and areola are removed, but the skin envelope is retained. This approach is often chosen when breast reconstruction is planned, as it provides a better aesthetic outcome.
- Nipple-Sparing Mastectomy: In nipple-sparing mastectomy, both the breast tissue and skin, as well as the nipple and areola, are preserved. This type of mastectomy is performed when the patient is considering breast reconstruction, and the nipple can be saved without compromising cancer treatment or recurrence risk.
- Subcutaneous (Nipple-Sparing) Mastectomy: This type of mastectomy is primarily performed for transgender individuals undergoing gender confirmation surgery. It preserves the nipple and areola and removes the breast tissue.
- Radical Mastectomy: This is an extensive procedure in which the entire breast, the underlying chest muscles (pectoralis major and sometimes minor muscles), and the lymph nodes are removed. Radical mastectomies are now rarely performed, as they have been largely replaced by less invasive approaches.
Your surgeon will determine the most appropriate type of mastectomy based on your specific circumstances, including the extent of the disease, your overall health, and your personal preferences.
Emotional Considerations
Emotional considerations play a crucial role in the experience of a mastectomy, as the procedure can have a significant impact on a person’s mental and emotional well-being. Understanding and addressing these emotions is vital for a person’s overall recovery and adjustment. Here are some of the emotional considerations that individuals may encounter before, during, and after a mastectomy:
- Grief and Loss: It’s entirely normal to experience feelings of grief and loss, not only for the physical loss of the breast(s) but also for the potential loss of a sense of femininity or attractiveness. It’s essential to allow yourself to mourn these losses and give yourself the time to heal emotionally.
- Anxiety and Fear: The period leading up to the mastectomy is often filled with anxiety and fear. Individuals may be anxious about the surgery, the potential for pain, and the unknowns of the recovery process. Fear of recurrence is also common, especially for those with breast cancer.
- Body Image Issues: A mastectomy can lead to changes in body image and self-esteem. It may take time to adjust to these changes and accept a new self-image. Seeking support from loved ones and counselors can help with body image issues.
- Depression: It’s not uncommon for individuals to experience depression after a mastectomy. Feelings of sadness, hopelessness, and a loss of interest in activities can be signs of depression. It’s crucial to seek help from mental health professionals if these feelings persist.
- Self-Esteem and Self-Worth: The surgery can affect a person’s self-esteem and self-worth. It’s important to remember that one’s value is not solely determined by physical appearance. You are still the same valuable person you were before the surgery.
- Social and Relationship Impact: Relationships with family, friends, and partners can be affected. Communicating openly with loved ones about your feelings and needs can help maintain and strengthen these relationships.
- Support System: Building a support system of friends, family, and support groups is essential. Sharing your experiences with others who have gone through similar situations can provide a sense of understanding and empathy.
- Post-Traumatic Stress: Some individuals may experience post-traumatic stress symptoms related to the mastectomy experience. If you’re having flashbacks, nightmares, or intrusive thoughts related to the surgery, it’s important to discuss this with a mental health professional.
- Counseling and Therapy: Consider seeking the support of a mental health professional or therapist. They can help you process your emotions and develop coping strategies to navigate the emotional challenges of a mastectomy.
- Self-Care: Prioritize self-care, which includes practicing mindfulness, relaxation techniques, engaging in activities that bring you joy, and taking time for yourself.
Remember that emotional healing takes time, and it’s okay to seek help and support. Every individual’s experience is unique, and there’s no one-size-fits-all approach to coping with the emotional aspects of a mastectomy. The key is to acknowledge and address your emotions, surround yourself with understanding and supportive individuals, and focus on your emotional well-being as part of your overall recovery. Your emotional resilience and strength can be as remarkable as your physical healing.
Reconstruction Options
Breast reconstruction is a significant consideration for individuals who have undergone a mastectomy. It is an elective surgical procedure that aims to restore the appearance of the breast and, in many cases, help improve a person’s self-esteem and body image. There are several breast reconstruction options to consider, and the choice depends on various factors, including the individual’s preferences, health, and the type of mastectomy performed. Here are some common breast reconstruction options:
- Implant-Based Reconstruction:
- Silicone Implants: Silicone breast implants are filled with a silicone gel that closely resembles the natural feel of breast tissue. They come in various shapes and sizes to suit individual preferences.
- Saline Implants: Saline implants are filled with sterile saltwater (saline) after insertion. These implants can be adjusted for size and symmetry as needed.
- Two-Stage Reconstruction: In this approach, a tissue expander is initially placed under the chest muscle to create a pocket for the implant. Over several months, the expander is gradually filled with saline to stretch the skin and muscle. Once the desired size is achieved, the expander is replaced with a permanent silicone or saline implant.
- Autologous Tissue (Flap) Reconstruction:
- TRAM Flap (Transverse Rectus Abdominis Muscle): This technique uses muscle, fat, and skin from the abdomen to reconstruct the breast. It can be a good choice for those who desire a more natural feel and appearance.
- DIEP Flap (Deep Inferior Epigastric Perforator): Similar to the TRAM flap, the DIEP flap uses abdominal tissue but preserves the abdominal muscles, making it a less invasive option.
- Latissimus Dorsi Flap: This procedure uses muscle, fat, and skin from the back, along with an implant, to reconstruct the breast. It is often used when there is insufficient tissue elsewhere for autologous reconstruction.
- Combination Procedures:
- Some individuals may opt for a combination of autologous tissue and implant reconstruction, depending on their specific circumstances.
- Nipple and Areola Reconstruction:
- After the initial reconstruction, a separate procedure can be performed to create a nipple and areola. This helps to complete the natural appearance of the breast.
- Fat Grafting (Lipofilling):
- Fat grafting is a technique that involves transferring fat from one part of the body (usually the abdomen or thighs) to the reconstructed breast. It can help improve contour and symmetry.
- Non-Reconstruction (Prosthetics):
- Some individuals choose not to undergo breast reconstruction. Instead, they may use external breast prostheses, which are wearable inserts designed to mimic the shape and feel of the natural breast.
It’s important to note that the choice of breast reconstruction method should be discussed in detail with a plastic surgeon and oncologist. Considerations include the individual’s overall health, the type of mastectomy performed, personal preferences, and the potential for future treatments or surgeries.
Breast reconstruction is a highly personalized decision, and what works for one person may not be suitable for another. Ultimately, the goal is to help individuals regain confidence and feel more comfortable with their bodies after a mastectomy. The specific method chosen should align with the individual’s unique circumstances and desires.
Post-Surgery Recovery
Recovery after a mastectomy is a critical phase in the journey toward physical and emotional healing. While the specific details of the recovery process can vary depending on the type of mastectomy and any additional procedures, here are some general guidelines for post-surgery recovery:
- Pain Management: You can expect some pain and discomfort after the surgery. Your healthcare team will provide you with appropriate pain medications. It’s essential to take these medications as prescribed and communicate any concerns or changes in pain to your healthcare provider.
- Drains: After a mastectomy, you may have surgical drains in place to remove excess fluid from the surgical site. Your healthcare provider will teach you how to care for these drains, including emptying them and measuring the fluid output. Keep accurate records and follow your healthcare team’s instructions regarding when the drains can be removed.
- Incision Care: Proper care of the incisions is crucial to prevent infection and promote healing. Follow your healthcare provider’s instructions for cleaning and dressing the surgical site. Keep the incisions clean and dry as directed.
- Physical Activity: During the initial recovery period, you’ll be advised to limit strenuous physical activity. It’s important to rest and allow your body to heal. However, you should also engage in gentle movements and exercises as recommended by your healthcare team to prevent stiffness and maintain range of motion.
- Emotional Support: Emotional recovery is a significant aspect of post-surgery healing. It’s common to experience a wide range of emotions, including grief, anxiety, and changes in body image. Seek emotional support from friends, family, and, if needed, mental health professionals. Support groups can also provide valuable insights and shared experiences.
- Follow-Up Appointments: Regular follow-up appointments with your healthcare provider are essential to monitor your healing and address any concerns. These appointments will help ensure that you are recovering as expected and can detect and address any complications or issues promptly.
- Lymphedema Management: Depending on the type of mastectomy and whether lymph nodes were removed, you may be at risk for lymphedema, a condition characterized by swelling in the arm or chest area. If necessary, your healthcare team will provide guidance on how to prevent and manage lymphedema.
- Nutrition and Hydration: Maintaining a balanced diet and staying well-hydrated are essential for recovery. Proper nutrition supports the healing process and overall well-being.
- Pain-Free Mobility: As you recover, work with your healthcare provider to gradually regain pain-free mobility and range of motion. Physical therapy or exercises may be recommended to help with this process.
- Scar Management: Over time, you may explore options for managing and minimizing the appearance of surgical scars, such as silicone gels or sheets, as recommended by your healthcare provider.
- Breast Reconstruction Planning: If you are considering breast reconstruction, discuss your options and timeline with your healthcare team. The timing and method of reconstruction can vary, so make informed decisions that align with your preferences and medical considerations.
Recovery after a mastectomy is a multifaceted process that involves both physical and emotional healing. Remember that everyone’s journey is unique, and the timeline for recovery can vary from person to person. Be patient with yourself, prioritize self-care, and lean on your support network as you navigate the challenges and triumphs of post-surgery recovery. Your resilience and determination will guide you toward a brighter, healthier future.
Disclaimer
This blog post is provided for informational purposes only and should not be considered as medical advice. Consult with your healthcare provider for personalized guidance and recommendations regarding mastectomy, recovery, and any related medical decisions.
Stay updated—subscribe now for informed empowerment!
Discover more from HUMANITYUAPD
Subscribe to get the latest posts sent to your email.

