Meniere’s Disease: Unraveling the Inner Ear Enigma
Meniere’s disease is a chronic and often debilitating condition that affects the inner ear, leading to a range of symptoms such as vertigo, hearing loss, and tinnitus. Named after the French physician Prosper Meniere, who first identified the condition in 1861, Meniere’s disease remains a challenging puzzle for both patients and healthcare professionals. In this blog post, we will explore the various aspects of Meniere’s disease, from its symptoms and causes to diagnosis and management strategies.
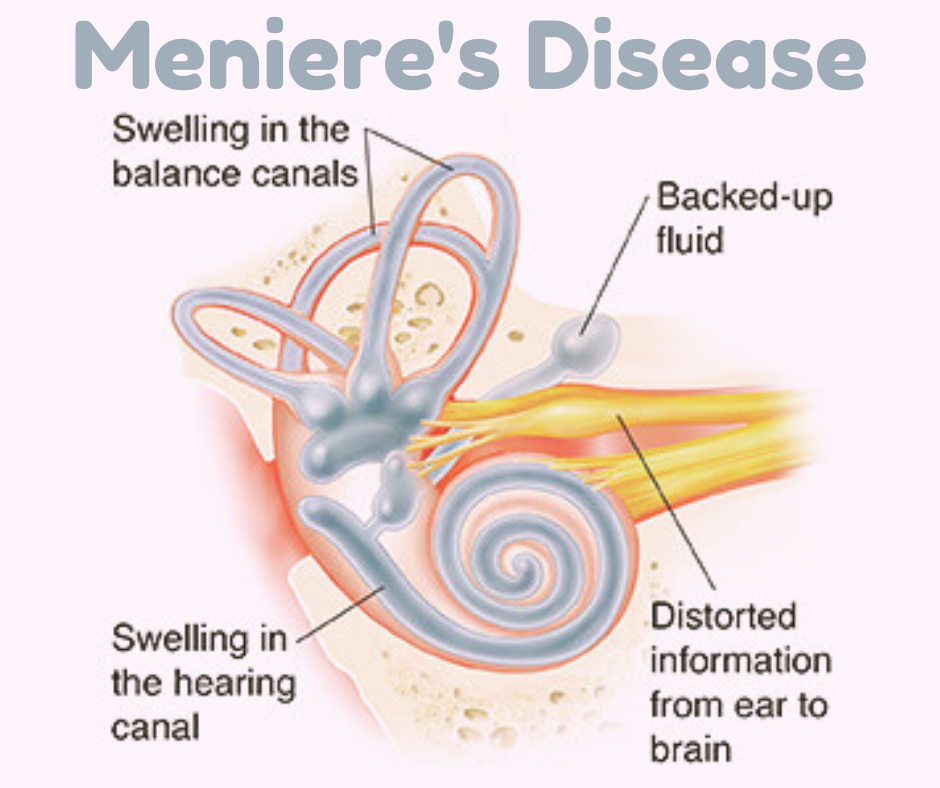
Understanding Meniere’s Disease
Meniere’s disease primarily impacts the inner ear, which plays a crucial role in maintaining balance and hearing. The condition is characterized by episodes of vertigo, a spinning sensation that can last for minutes to hours, accompanied by other symptoms like hearing loss, tinnitus (ringing in the ears), and a feeling of fullness or pressure in the affected ear.
Symptoms of Meniere’s Disease
Meniere’s disease is characterized by a combination of symptoms that primarily affect the inner ear. The severity and frequency of these symptoms can vary from person to person. The classic symptoms of Meniere’s disease include:
1. Vertigo:
- Description: Intense, unpredictable episodes of dizziness.
- Sensation: A spinning or whirling sensation.
- Duration: Episodes can last anywhere from a few minutes to several hours.
- Accompanied by: Nausea, vomiting, and a general unsteadiness.
2. Hearing Loss:
- Nature: Hearing loss in Meniere’s disease is typically fluctuating, affecting one ear initially.
- Progression: Over time, hearing loss may become more pronounced and can involve both low and high frequencies.
- Permanent Damage: In some cases, hearing loss may become permanent.
3. Tinnitus:
- Type: Persistent ringing, buzzing, hissing, or roaring sounds in the affected ear.
- Intensity: Tinnitus can vary in intensity and may become more noticeable during episodes of vertigo.
- Impact: The continuous presence of these sounds can be distressing for individuals with Meniere’s disease.
4. Aural Fullness:
- Sensation: A feeling of fullness, pressure, or blockage in the affected ear.
- Timing: Aural fullness may occur before, during, or after episodes of vertigo.
5. Vestibular Symptoms:
- Imbalance: Individuals with Meniere’s disease may experience imbalance and difficulty maintaining posture.
- Sensitivity to Motion: Increased sensitivity to motion, making activities like walking or driving challenging during and after vertigo episodes.
6. Cognitive Symptoms:
- Concentration Issues: The unpredictability of symptoms can lead to difficulties concentrating and focusing on tasks.
- Fatigue: Managing the physical and emotional toll of Meniere’s disease can result in fatigue.
Causes and Triggers
While the exact cause of Meniere’s disease remains unclear, several factors may contribute to its development. These include:
1. Fluid Imbalance:
- Description: Changes in the fluid volume and composition within the inner ear.
- Impact: Disruptions in the delicate balance of fluids in the inner ear can affect its function, leading to symptoms like vertigo and hearing loss.
2. Genetic Predisposition:
- Family History: Meniere’s disease can sometimes run in families, suggesting a genetic component.
- Inheritance: While not fully understood, there may be a hereditary predisposition to the condition.
3. Vascular Issues:
- Poor Blood Flow: Problems with blood flow to the inner ear could contribute to the development of Meniere’s disease.
- Ischemia: Reduced blood supply may lead to damage in the inner ear structures.
4. Autoimmune Factors:
- Immune System Response: Some researchers propose that an autoimmune response may play a role in Meniere’s disease.
- Inflammation: Autoimmune reactions could cause inflammation in the inner ear, contributing to symptoms.
5. Allergies:
- Connection: Allergic reactions and sensitivities may exacerbate symptoms or act as triggers for Meniere’s disease.
- Inflammation: Allergies could contribute to inflammation in the ear, affecting its function.
6. Infections:
- Viral Infections: Prior viral infections, especially those affecting the inner ear, may contribute to the development of Meniere’s disease.
- Bacterial Infections: Infections affecting the ear can potentially lead to inner ear damage.
7. Migraines:
- Association: Some individuals with Meniere’s disease also experience migraines.
- Shared Mechanisms: Shared vascular and neurological mechanisms between migraines and Meniere’s disease may contribute to symptoms.
8. Environmental Factors:
- Lifestyle Factors: Factors such as stress, smoking, and dietary choices may influence the severity and frequency of Meniere’s disease symptoms.
- Salt Intake: Excessive salt intake can contribute to fluid retention and may worsen symptoms in some individuals.
9. Physical Trauma:
- Head Trauma: In some cases, head injuries or trauma to the ear may be associated with the onset of Meniere’s disease symptoms.
Diagnosis
Diagnosing Meniere’s disease can be challenging due to the absence of specific diagnostic tests. Healthcare professionals typically rely on a combination of medical history, physical examination, and specialized tests to make an accurate diagnosis. Here are the key steps involved in diagnosing Meniere’s disease:
1. Medical History:
- Symptom Review: A detailed discussion about the nature, frequency, and duration of symptoms, including vertigo, hearing loss, tinnitus, and aural fullness.
- Triggers: Identifying potential triggers or patterns associated with symptom onset.
2. Physical Examination:
- Otoscopic Examination: A visual inspection of the ear canal and eardrum to rule out other ear conditions.
- Neurological Examination: Assessing balance and coordination to identify any neurological issues.
3. Audiometry:
- Pure-Tone Audiometry: Evaluating hearing acuity to detect any hearing loss.
- Speech Audiometry: Assessing the ability to hear and understand spoken words.
4. Vestibular Testing:
- Electronystagmography (ENG): Measures involuntary eye movements to assess the function of the vestibular system.
- Videonystagmography (VNG): Uses video recording to track eye movements during specific tests.
5. Imaging Studies:
- Magnetic Resonance Imaging (MRI): In some cases, an MRI may be performed to rule out other conditions affecting the inner ear or the brain.
6. Electrocochleography (ECochG):
- Purpose: Measures electrical potentials generated in the inner ear in response to sound stimuli.
- Detection of Endolymphatic Hydrops: This test may help identify increased fluid levels in the inner ear, a characteristic associated with Meniere’s disease.
7. Other Tests:
- Posturography: Evaluates balance and postural stability.
- Blood Tests: To rule out systemic conditions that may contribute to symptoms.
8. Diagnostic Criteria:
- Duration and Frequency: The diagnosis often involves considering the duration, frequency, and severity of episodes over time.
- Exclusion of Other Conditions: Since there is no definitive test for Meniere’s disease, it’s crucial to rule out other conditions that may mimic its symptoms.
9. Consistent Pattern of Symptoms:
- Episodic Nature: Meniere’s disease is characterized by episodic bouts of symptoms rather than constant symptoms.
- Association of Symptoms: The simultaneous occurrence of vertigo, hearing loss, tinnitus, and aural fullness during episodes supports the diagnosis.
10. Monitoring Over Time:
- Observation: Meniere’s disease is often diagnosed based on the observation of a consistent pattern of symptoms over time.
Management and Treatment
While there is no cure for Meniere’s disease, various treatment strategies aim to manage symptoms and improve the quality of life for affected individuals. These may include:
Lifestyle Modifications:
- Dietary Changes:
- Reduced Salt Intake: Lowering salt intake can help manage fluid retention in the inner ear, potentially reducing the severity of symptoms.
- Hydration:
- Adequate Fluid Intake: Maintaining proper hydration can support overall health and potentially contribute to fluid balance.
- Avoiding Triggers:
- Identifying and Avoiding Triggers: Identifying and minimizing exposure to factors that may trigger episodes, such as stress, caffeine, and certain foods.
Medications:
- Diuretics:
- Purpose: Diuretic medications help reduce fluid retention, potentially alleviating symptoms.
- Examples: Hydrochlorothiazide, triamterene.
- Vestibular Suppressants:
- Purpose: Medications that suppress vestibular function, helping to control vertigo.
- Examples: Meclizine, diazepam.
- Anti-nausea Medications:
- Purpose: Addressing nausea and vomiting associated with vertigo episodes.
- Examples: Promethazine, ondansetron.
Hearing Aids:
- Hearing Amplification:
- Hearing Aids: For individuals with hearing loss, hearing aids can help improve communication and quality of life.
Cognitive Behavioral Therapy (CBT):
- Emotional Support:
- CBT: Therapy can help individuals cope with the emotional impact of Meniere’s disease, including anxiety and depression.
Physical Therapy:
- Vestibular Rehabilitation:
- Exercises: Specific exercises can improve balance and reduce the impact of vertigo on daily activities.
Invasive Treatments:
- Intratympanic Steroid Injections:
- Purpose: Injections of steroids into the middle ear to reduce inflammation and control symptoms.
- Endolymphatic Sac Decompression Surgery:
- Purpose: Creating a shunt to drain excess fluid from the inner ear, potentially reducing symptoms.
- Vestibular Nerve Section or Labyrinthectomy:
- Purpose: Surgical procedures reserved for severe cases to disrupt signals causing vertigo.
Monitoring and Follow-up:
- Regular Check-ups:
- Follow-up Appointments: Regular monitoring with healthcare professionals to assess symptom management and adjust treatment plans as needed.
- Patient Education:
- Understanding the Condition: Education about Meniere’s disease, its course, and available treatments is crucial for managing expectations and optimizing coping strategies.
It’s important to note that the effectiveness of treatments can vary among individuals, and a personalized approach is often necessary. As Meniere’s disease is a chronic condition, management may involve ongoing adjustments to accommodate changes in symptoms and overall health. Individuals with Meniere’s disease are encouraged to work closely with their healthcare team to develop a comprehensive and tailored treatment plan that addresses their specific needs and concerns.
Disclaimer
The information provided in this blog post is for informational purposes only and should not be considered as medical advice. It is not intended to replace consultation with a qualified healthcare professional. If you suspect you have Meniere’s disease or are experiencing related symptoms, it is essential to consult with a healthcare professional for a thorough evaluation and appropriate diagnosis. Treatment plans should be tailored to individual needs, and any decisions regarding medical care should be made in consultation with a qualified healthcare provider.
Stay updated—subscribe now for informed empowerment!

